In several recent posts, I argued that most of us aren't getting enough choline, and that the disappearance of choline-rich foods like liver and egg yolks from the modern diet is likely responsible for the silent epidemic of fatty liver disease that may be afflicting 70-100 million Americans. If you missed them, you can find them here:
Does Your Liver Look Like an Eskimo's Dinner? Fatty Liver Is a Silent Epidemic
Does Choline Deficiency Contribute to Fatty Liver in Humans?
In this post, I'll try to outline what we know about how to get enough choline. And I'll share some surprising insights about the value of spinach, beets, and wheat, with a little discussion of what I'll call “The Wheat Paradox.”
Choline in Foods — It's All About the Organs and Eggs
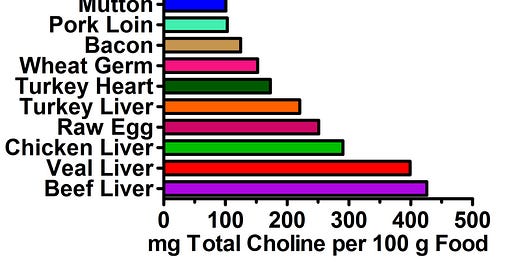
First, let's take a look at where we can get choline from. The following data is taken from the USDA database (1). Clearly, liver and eggs top the chart.
Unless stated otherwise, the values are for foods cooked, but without added fat. Although not shown, most other organ meats probably rank pretty high, especially brain and kidney.
Interestingly, wheat germ shows up on the list amidst a bunch of animal foods. This, however, is not the “Wheat Paradox.” It's just the tip of the iceberg. But more on that below.
Lots of other foods contain smaller amounts of choline. Here are some of the better ones:
Meats, seafood, and nuts tend to be decent sources of choline, but vegetables are widely variable. Boiled broccoli, cauliflower, and brussels sprouts have quite a bit of choline, but boiled kale has hardly any. In general, milk and fruit tend to lag further behind the vegetables. Spices are often decent sources of choline, but are usually used in small amounts.
Clearly, none of these foods come anywhere near organ meats and eggs. Liver and eggs, for example, have ten times more choline than most vegetables!
By far and away, most of the choline in these foods is found as phophatidylcholine, a membrane-bound phospholipid. As a result, it's found in the yolk of the egg and not in the white. A 100-gram serving of egg yolk has 683 mg of choline, whereas a similar serving of egg white has only 1.1 mg. For an equal amount of each, then, you'd get three times more choline out of your eggs if you threw away the whites.
I haven't found any evidence that heating foods affects the bioavailability of choline. If you know of any, please post it in the comments section.
Our next question, then is, how much choline do we actually need? Do we really need to eat egg yolks and liver every day?
The Impossible Question
Unfortunately, trying to estimate how much choline we need is almost impossible for three reasons: 1) there's very little scientific evidence in humans that can be used to justify a particular intake, 2) the choline requirement is dependent on the intake of several other vitamins, 3) the choline requirement depends on certain genetic variations, and 4) the choline requirement is dependent on the intake of several energy sources, such as sugar, alcohol, and fat. Thus, even if we look to traditional diets, we must attempt to unravel all of these interacting factors.
Nevertheless, there's good reason to think that the choline requirements of both lab rats and humans have been grossly underestimated.
Lab Rats Are Deficient in Choline

As I pointed out in “The Sweet Truth About Liver and Egg Yolks,” choline is capable of completely protecting lab animals against fatty liver induced by sugar, alcohol and fat. Yet the most common dietary models of fatty liver disease — besides choline deficiency — use high intakes of sugar, alcohol, or fat to induce the disease. This clearly suggests that choline provided by standard rodent diets is insufficient to allow the animals to deal with these energy sources.

The other piece of evidence relates to brain development. As I pointed out in my 2007 Wise Traditions lecture and article on pregnancy nutrition, “Vitamins For Fetal Development — From Conception to Birth,” pregnant rat moms fed three times their ordinary choline intake give birth to rat babies with some remarkable lifelong brain-boosting benefits. They have a 30 percent increase in visuospatial and auditory memory that lasts through their lives; they grow old without developing any age-related senility; they are protected against the assaults of neurotoxins; they have an enhanced ability to multi-task; and they have a much lower rate of interference memory. Interference memory is when a past memory interferes with an immediate memory — for example, when a past memory of where you parked your car interferes with your ability to find it when you exit the store.
The pregnant rat moms consumed this massive dose of choline during the period of gestation in which the choline-based neurons in the brain develop. In humans, this period of development corresponds to pregnancy and to the first four years of a child's life. Regardless of whether this enormous brain-boosting effect transfers over to humans, the fact that rats get such a huge benefit from increasing their choline intake so enormously very much supports the idea that current intakes are way too low.
To the Clinical Trial We Go, How Much Choline Humans Need Nobody Knows
For humans, the evidence about our choline requirement was so limited in 1998 that the Institute of Medicine had to set an “adequate intake (AI)” rather than an RDA. An AI is basically the “let's make a wild guess” version of the RDA. You can read the report here (2).
The AI is 550 mg/day for men and 425 mg/day for women. It assumes an average male weighs 76 kg or 168 pounds, and adjusts the male requirement downward for the female requirement as an adjustment for average bodyweight. It increases to 450 mg/day for pregnant women and 550 mg/day for nursing women. The increases are based on the typical concentration of choline in a fetus or in mother's milk. Since there's no reason to think “average” is best, the increases for pregnancy and lactation are basically meaningless.
All these numbers are based on the AI for adult males. This is taken from a single study (3) that successfully used 500 mg/day to suppress the increase in liver enzymes that occurred in healthy humans eating a choline-deficient diet. This is almost certainly lower than the true requirement for choline, however. “Liver enzymes,” or aminotransferases, are enzymes that spill out of liver cells into the bloodstream when liver cells start dying. This can happen as a result of fatty liver, but only when it progresses to a certain stage.
About 8% of Americans have elevated liver enzymes, roughly a third of which can be explained by known causes such as alcohol, iron overload, or hepatitis viruses (4). But as many as 30% of Americans may have fatty liver (5), and 80% of them have liver enzymes within normal limits (6). For the final proof in the pudding, out of ten women who developed liver problems when they were put on an experimental choline-deficient diet, nine of them developed fatty liver and only one of them developed elevated liver enzymes (7).
Thus, the choline requirement is almost certainly more than 500 mg/day. There are virtually no solid studies in the general population, however, that have randomized people to multiple different choline intakes and measured an important health outcome, which is what would be needed to establish a solid choline requirement.
Once recent exception to this rule (8) showed that 1100 or 2200 mg/day of choline protected against the DNA damage that otherwise occurred in people consuming 300 or 550 mg, but this study was very small and was conducted in men who were restricted to the RDA of folate, and who thus had declining folate status through the study. As we'll see below, the choline requirement depends on the intake of folate and a number of other nutrients.
The Choline Requirement Is Dependent on Intakes of Folate, B12, B6, and Betaine
Another reason it's almost impossible to come up with an exact amount of choline we should consume is because choline arrives at an intersection in the methylation pathway where it crosses paths with folate, vitamin B12, vitamin B6, and betaine. Here's a simplified chart showing this pathway:
As we can see from the chart, methionine is a critical amino acid used for the generation of SAM, which is in turn used for the methylation of proteins, DNA and other substances. Methylation is critical to the regulation of gene expression and the stability of our DNA, but it's also the process that we use to make choline! That's right, the PEMT enzyme uses SAM to make phosphatidylcholine, a choline-containing phospholipid that can later be broken down to free choline. For more information on the PEMT enzyme, see my post, “Does Choline Deficiency Contribute to Fatty Liver in Humans?”
Whenever SAM methylates another molecule, it generates SAH and then homocysteine. In all cells, homocysteine can be turned back into methionine to start the process all over again with the help of vitamin B12 and folate. In the liver, when the methylation process is proceeding adequately, vitamin B6 gets rid of any extra homocysteine by turning it into cysteine. The cysteine can then be used to make glutathione, the main antioxidant of the cell and one of the liver's principal detoxfication tools. For more on glutathione, see my post over at WestonAPrice.Org, “The Biochemical Magic of Raw Milk and Other Raw Foods: Glutathione.”
The liver and kidney can also use choline to make betaine, which can substitute for folate and B12 in the regeneration of methionine through a completely different enzymatic pathway. Betaine is also important to regulating osmotic pressure in the kidney.
Thus, folate, vitamin B12, B6, and betaine can spare choline, but only methionine can be used to make choline. The B vitamins and betaine can thus fulfill choline's role in methylation, at least in the liver and kidney, but only methionine can provide the choline needed to export liver fat, to serve as a neurotransmitter, or to make our cell membranes work properly. As I pointed out in “Does Choline Deficiency Contribute to Fatty Liver in Humans?,” studies conducted thus far suggest that the vast majority of our population may have at least one not-so-effective gene for making choline from methionine.
To make even more of a mess of this, the PEMT enzyme actually creates homocysteine in the process of creating choline! So, if your PEMT engine is running nice and smoothly, you can make your own choline, but you still need more betaine and B vitamins to neutralize the homocysteine that's generated in the process. If your PEMT engine is working like this, however…
… well, then, you've got another problem. If PEMT isn't using up your methionine to make choline, the methionine is just going to go further on down that pathway shown above and make more homocysteine anyway!
Thus, although having a PEMT gene that Uncle Buck would surely envy might lower our choline requirement, consuming lots of methionine won't help us at all. In fact, extra methionine just gives us more homocysteine and thereby increases our need for choline, betaine, folate, B12, and B6.
As I previously pointed out in my 2007 pregnancy nutrition article, the interplay between all these nutrients as well as some other amino acids is one reason we don't want to load up on lean muscle meats. Rather, we should balance muscle meats with skin, bones, organs, and leafy vegetables.
While extra methionine isn't such a great idea, studies clearly support an interaction between the B vitamins and choline and show that B vitamins, betaine, and choline can all substitute for each other in order to support the methylation pathway (9, 10, 11, 12, 13). Thus, whether we need to actually eat choline or just eat B vitamins and betaine instead will be largely determined by how great our PEMT enzyme works.
And this, dear friends, leads us to “The Wheat Paradox.”
The Mighty Mighty Betaine and The Wheat Paradox
In the comments of “Does Choline Deficiency Contribute to Fatty Liver in Humans?” blogger and commenter Ned Kock suggested that the choline connection may be able to resolve a number of apparent paradoxes. Indeed, it could certainly resolve contradictory findings about whether common energy stores like sugar, alcohol, and fat are bad for us, since these substances clearly increase the need for choline. But our buddy betaine is taking a big elephant in the room for a ride, and the elephant's name is Wheat.
We are all, of course, awaiting with baited breath Denise Minger's long-anticipated wheat post, in which she will reveal some plausible mechanisms by which wheat could contribute to the risk of heart disease. But Denise also uncovered the curious case of the Tuoli, who lived largely off wheat and dairy, but had reasonably low rates of cardiovascular and other diseases. Likewise, the inhabitants of Crete live largely off wheat and dairy. Although they do have some heart disease, studies in the 1960s showed that the rates were very low by Western standards, especially for a population where half the men smoked (15).
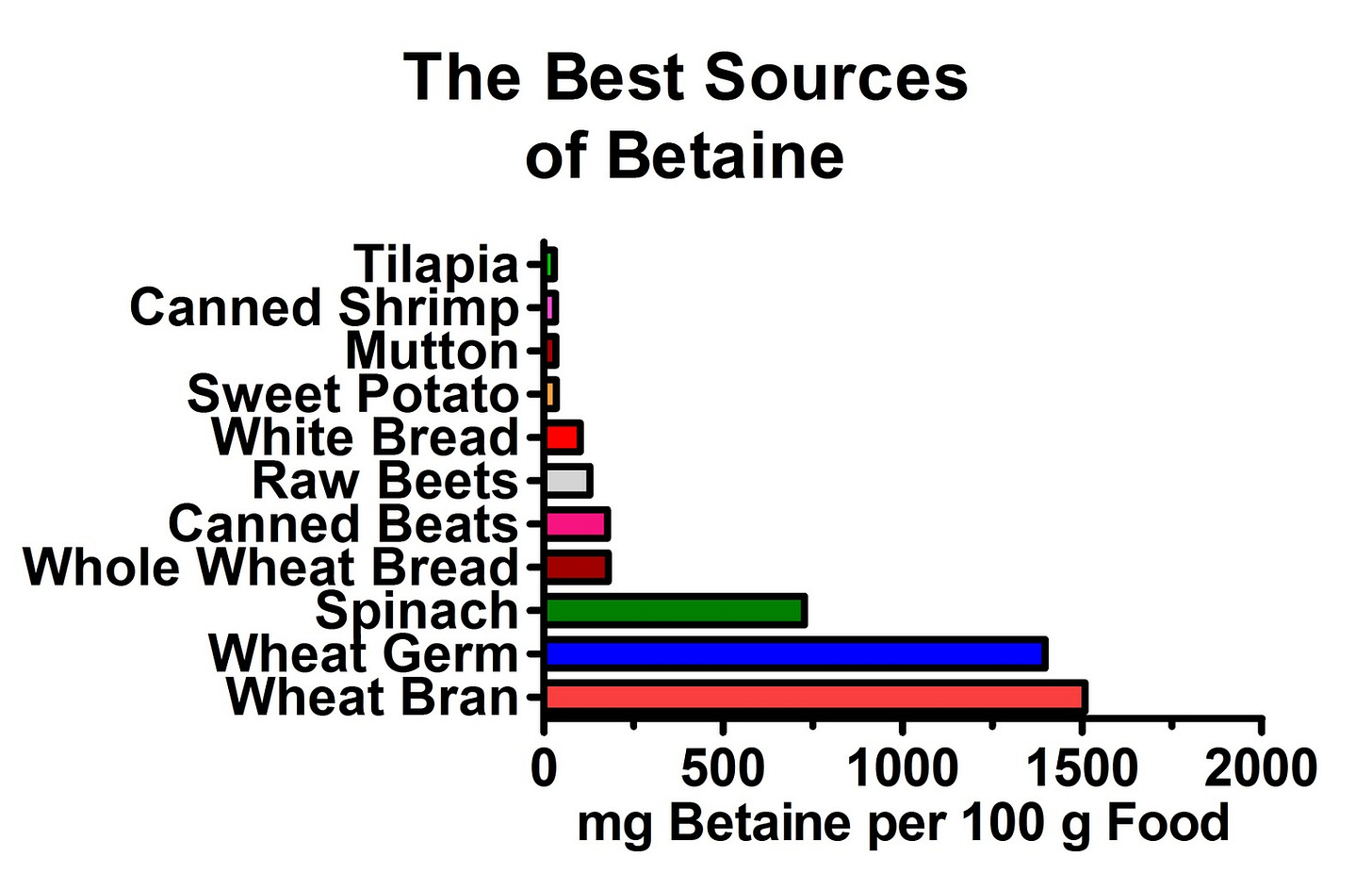
As it turns out, by far and away the the best sources of betaine (1) are wheat and spinach:
The betaine is especially abundant in the germ and bran of the wheat, but wheat is such a great source that even white bread of all things has a decent amount! By contrast, virtually every other food has such a puny amount of betaine in it that it couldn't climb onto this chart even if the very existence of the world depended on it.
Clearly, wheat offers a major advantage to someone with a low intake of eggs and organ meats, and spinach would offer a similar benefit on a gluten-free diet. In fact, spinach is much richer in betaine than whole wheat.
The choline connection may thus provide resolution to a number of paradoxes, including one that Ned pointed out, that the French consume plenty of white bread. It's the red wine, the red wine, the red wine! Perhaps. But eating liver is likely to protect against some of the nasty effects of eating sweets, and even white bread has the surprising saving grace of providing some betaine in addition to the otherwise nutrient-depleted package of toxic junk it provides.
As pointed out above, however, we can't be quick to assume that betaine can replace choline in everyone. As pointed out above, genetic variation in the PEMT gene will most likely make or break the success of such a replacement.
Genes and the Choline Requirement
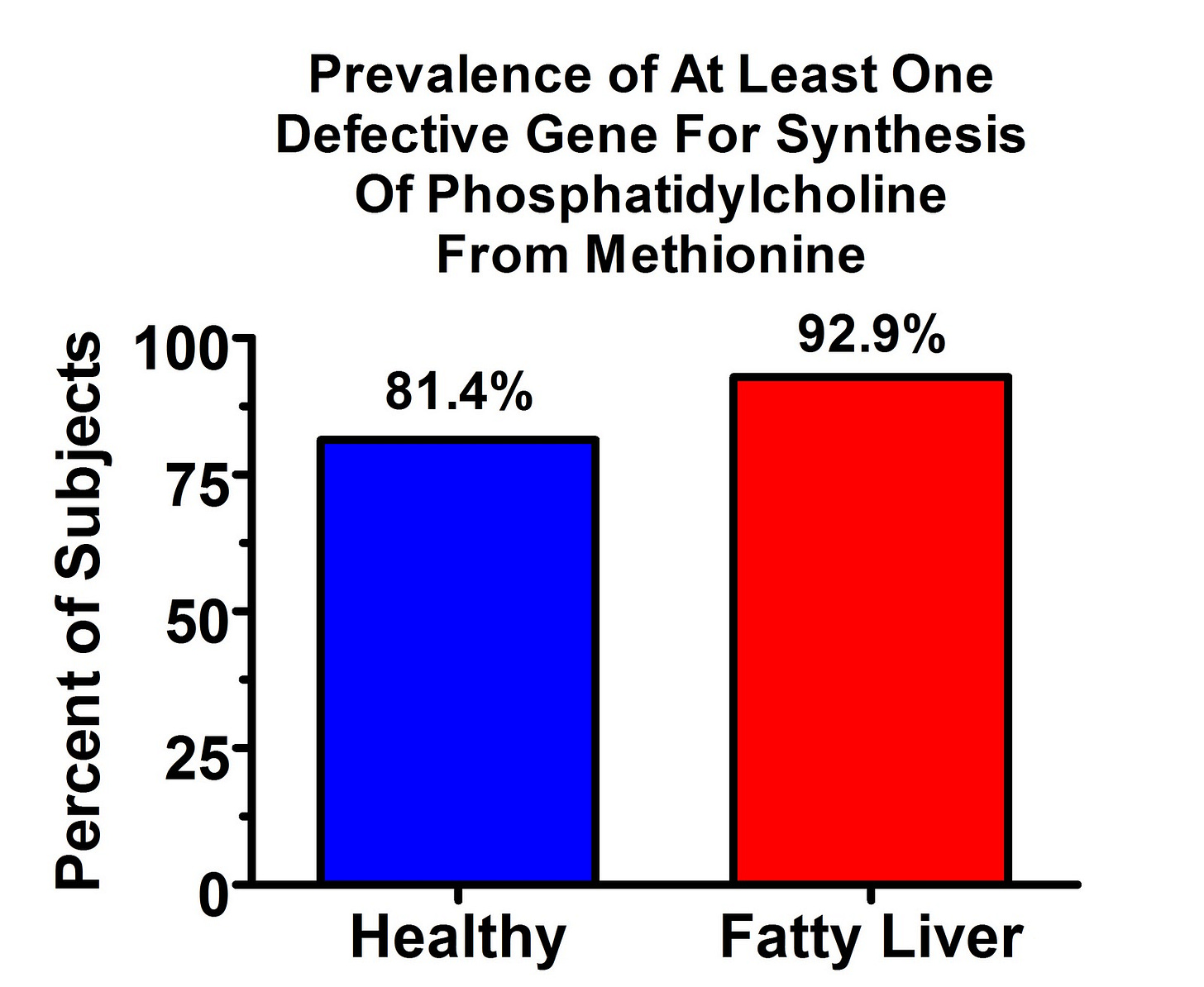
As I pointed out in “Does Choline Deficiency Contribute to Fatty Liver in Humans?,” studies conducted thus far suggest that the vast majority of people in our population may have a not-so-effective version of the PEMT gene. Consider this graph from an American study (16):
Even among healthy controls, the prevalence of at least one “defective” version (“defective” compared to the other version) is over 80%.
Such studies (16, 17, 18) have involved anywhere from fewer than 100 people to over 3000 people, have been conducted in North Carolina and Long Island, and have represented Caucasians, African-Americans, Asians, Native Americans, and other heritages. They have consistently shown the prevalence of at least one copy of the less effective gene in 75-88% of the population. Nevertheless, there is likely to be considerable variation between ethnic groups, and the high prevalence probably primarily reflects the Caucasians and possibly African Americans that have been represented in these studies to greater extents than other groups.
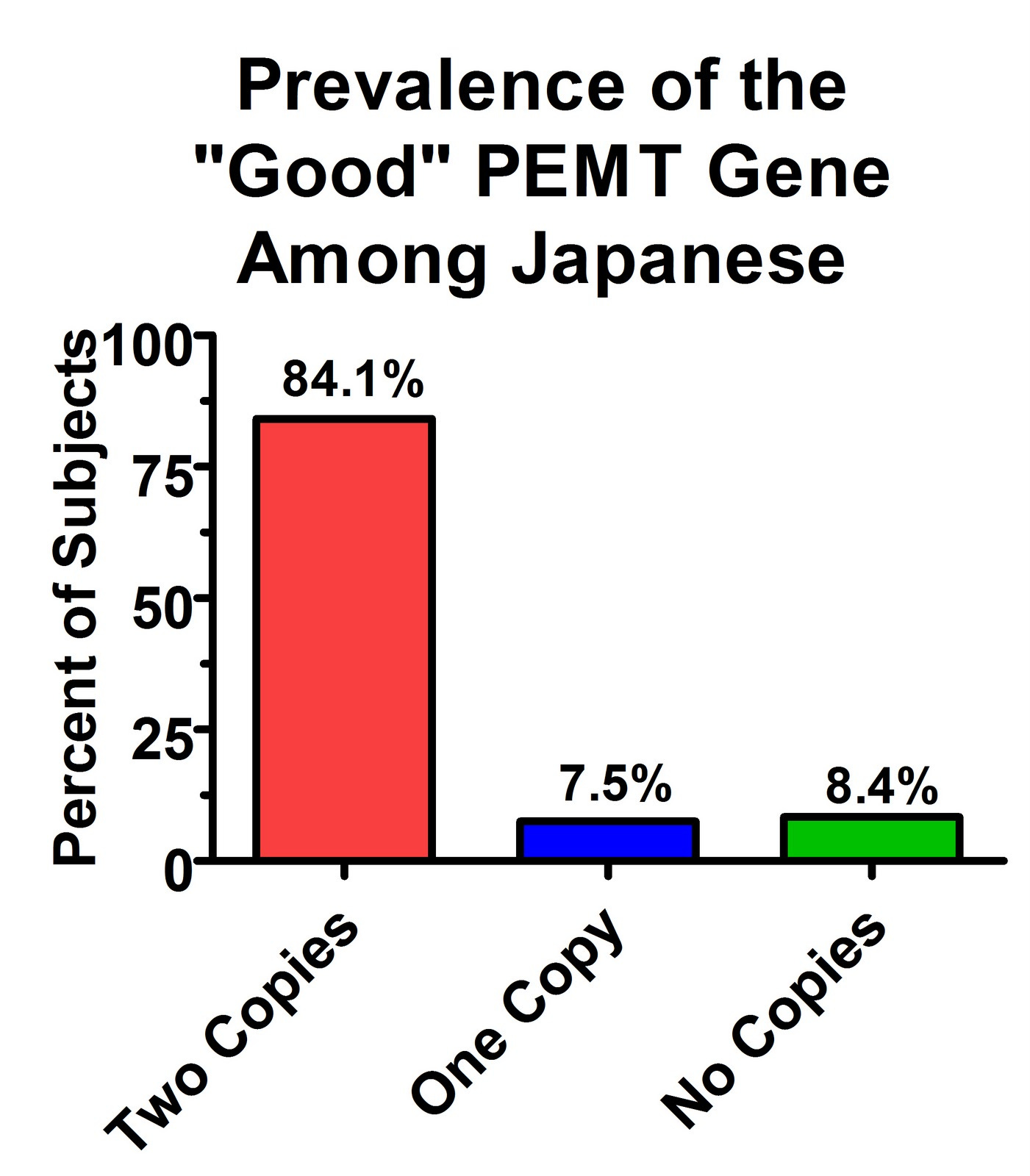
In the comments of “Does Choline Deficiency Contribute to Fatty Liver in Humans?,” Ed suggested that cultures with more plant-based and less organ meat-based diets might have higher prevalences of the more effective PEMT gene.
There aren't many studies on this available, but there's certainly large variation between populations. Here's the prevalence found in a recent Japanese study (19):
Whereas most Americans may have at least one copy of the less effective gene, most Japanese may have two copies of the more effective gene and none of the less effective gene.
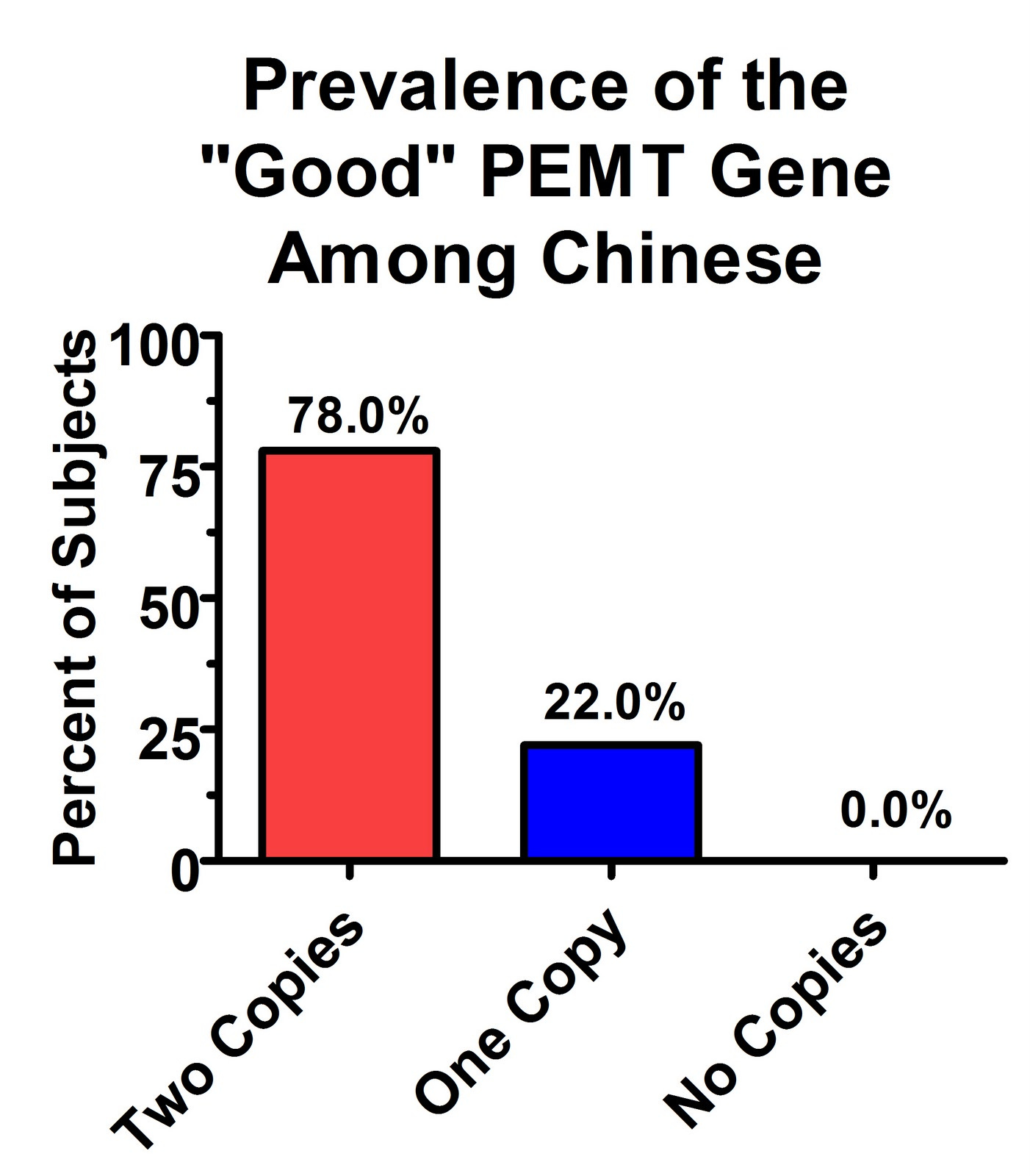
Similar results were found in a recent Chinese study (20):
Thus, it is quite plausible that some populations have very high prevalences of the “good” version of this gene, which allows them to make their own choline from methionine for the export of liver fat, to use as a neurotransmitter, and to use in cell membranes. Meanwhile, they could neutralize the homocysteine generated in the production of choline with high intakes of betaine, folate, and vitamins B6 and B12.
Aye! So How Much Choline Are You Saying We Need???
In conclusion, rather than declaring how much choline people need to eat, we can much better support Ned Kock's idea that the choline connection will, when viewed properly, resolve lots of apparent paradoxes.
Not everyone needs a lot of choline. People with two copies of the awesome ‘possum version of the PEMT gene may get by with very little choline but with very high intakes of B vitamins and betaine. People with one or more of the not-so-hot version of this gene may need lots of organ meats and egg yolks to keep their liver from looking like an Eskimo's dinner.
In America, at least, it would appear that lots of us need lots of egg yolks and liver.
Read more about Chris Masterjohn, PhD, here.
Join the Next Live Q&A
Have a question for me? Ask it at the next Q&A! Learn more here.
Subscribe
Subscribe or upgrade your subscription here.
Join the Masterpass
Masterpass members get access to premium content (preview the premium posts here), all my ebook guides for free (see the collection of ebook guides here), monthly live Q&A sessions (see when the next session is here), all my courses for free (see the collection here), and exclusive access to massive discounts (see the specific discounts available by clicking here). Upgrade your subscription to include Masterpass membership with this link.
Learn more about the Masterpass here.
Take a Look at the Store
At no extra cost to you, please consider buying products from one of my popular affiliates using these links: Paleovalley, Magic Spoon breakfast cereal, LMNT, Seeking Health, Ancestral Supplements. Find more affiliates here.
For $2.99, you can purchase The Vitamins and Minerals 101 Cliff Notes, a bullet point summary of all the most important things I’ve learned in over 15 years of studying nutrition science.
For $10, you can purchase The Food and Supplement Guide for the Coronavirus, my protocol for prevention and for what to do if you get sick.
For $29.99, you can purchase a copy of my ebook, Testing Nutritional Status: The Ultimate Cheat Sheet, my complete system for managing your nutritional status using dietary analysis, a survey of just under 200 signs and symptoms, and a comprehensive guide to proper interpretation of labwork.






Hi, you're egg calculator gave me recommendations. I'm trying 50% choline and 50% TMG. I found a study that showed choline from eggs were absorbed 4 times higher than the same amount from the choline in supplements. That's a big difference. I'm not sure if you're recommendation is the value I'd get from actual eggs or the supplement. BTW I feel amazing since starting choline and TMG.
Dr. Masterjohn, I'm a 22-year-old who has been devastated by chronic health issues following ciprofloxacin toxicity, leading to severe neuropathy and mitochondrial dysfunction over the past 2 years. My case is complicated by gallbladder dysfunction (not showing up on tests but with persistently yellow stool; unresponsive to ox bile and digestive supplements), severe oxalate toxicity (causing thyroid issues and elevated molybdenum, selenium, and iodine), and paradoxical reactions to B vitamins, despite extensive supplementation and intervention.
I’ve tried everything I can but continue to deteriorate. I believe my case is unique and complex, likely involving bioenergetic blocks and mineral dysregulation that few practitioners have the expertise to address. I am confident that healing is possible, as some interventions have shown temporary effectiveness before abruptly stopping. This indicates that recovery is certainly possible, but I realize I need world-class expertise to truly overcome these challenges and cannot seem to do this on my own. Your work has truly been a beacon of hope for me, and I am desperate for your guidance. Could you please consider offering me a consultation or a place in your Bio Opt program? I have been on the waiting list for over a year and am willing to take any opportunity. I am ready to travel immediately from the EU to the US (I already have a visa).
I feel like my young life is slipping away from me. I just want to live a normal life again. I hope you receive this message in good health, and I sincerely appreciate your consideration. Thank you for all that you do.
I've created a special email for this purpose: maxforchrismasterjohn@gmail.com