Biotin Causes a Multitude of False Lab Tests | Here is What to Do
High-dose biotin supplements can cause a multitude of false lab tests, masking recent heart attacks, pregnancies, or allergies, giving false signals about tumors, and far more. Here is what to do.
I am not a medical doctor and this is not medical advice. Please see the full disclaimer at the bottom.
Biotin is a B vitamin, also known as vitamin B7. It plays a critical role in energy metabolism, neurological health, and blood sugar stability. It is widely used as an over-the-counter supplement for hair, skin, and nail health, and is currently being studied in very high doses as a treatment for multiple sclerosis.
Despite the many benefits of biotin, high-dose biotin supplements can cause false signals on a multitude of lab tests. This has the potential to mask recent heart attacks, pregnancies, or allergies; to misdiagnose thyroid conditions; to give false signals about the presence or progression of tumors; to falsely raise vitamin D, B12, and folate levels; to falsely alter many hormone levels; to generate false positives for HIV and hepatitis; and it has led to at least one unnecessary surgery and possibly to a death.
In this article, we examine the nature and scope of the problem, and what we need to do to deal with it.
What Is a “High Dose” of Biotin?
There is no officially recommended intake for biotin, but the current guidelines used in the United States took the average intake of American infants, adjusted it upwards based on bodyweight, and concluded that 30 micrograms per day “should be adequate” to prevent deficiency in adults. This is the adequate intake, or AI, which is set by the Food and Nutrition Board of the National Academy of Medicine when there is not enough evidence to set a recommended dietary allowance, or RDA. The FDA has, in turn, adopted this figure to set its Daily Value for biotin at 30 micrograms as well. The FDA’s Daily Values are used for the labeling on packaged foods and supplements.
In High Protein? You Need More Biotin, I made the case that 30 micrograms per day is not enough for adults, and that many people need 150-300 micrograms per day, depending on how much protein they eat. My simple food-based recommendations for getting enough biotin are found in my Cliff Notes (free for Masterpass members here). Incidentally, 300 micrograms was used as the FDA’s Daily Value until it was changed to 30 in 2016.
Many people are using supplements providing far higher doses. A milligram is 1000 micrograms, and many supplements contain between 1 and 300 milligrams. This is between 1,000 and 300,000 micrograms, and it ranges from 3.3-10,000 times the values thought to be adequate in the various sources I cited above. This is the range that will be referred to as “high-dose” biotin throughout this article.
How Common Are High-Dose Biotin Supplements?
The most recent comprehensive data for the United States show that the number of people using biotin supplements providing at least one milligram per day increased 28-fold between 1999 and 2016. In absolute terms, the use of high-dose biotin increased from 0.1% to 2.8%.
Data for supplements providing 5 milligrams or more were not available until 2007. Between then and 2016, use increased 7-fold from 0.1% to 0.7%.
The prevalence was highest in women over the age of 60, 7.4% of whom used biotin at a dose of at least one milligram per day, and 2.3% of whom used a dose of at least 5 milligrams per day.
In 2017, the Mayo Clinic conducted a survey of 4,000 patients who came in for routine bloodwork. 48.6% of these people responded. Among them, 7.7% reported taking biotin supplements. The respondents overall were 49-72 years old. Biotin users were three times more likely to be female. Nearly a third of them did not know what dose they were taking. Of the rest, over 96% took more than 1 milligram per day, and the most common doses were 1, 5, and 10 milligrams per day.
A collaborative study done by Weill Cornell Medical College and UCLA’s Department of Medicine was originally made available in 2020 and published in final form this year. In a sample heavily biased towards dermatologists (81.9% of respondents), they surveyed 149 physicians and found that just under 43.9% of them recommended biotin to their patients, most often for hair and nail disorders. The dermatologists were 2.6 times more likely to recommend biotin than other physicians.
While 62.5% of the physicians knew that biotin can interfere with thyroid function tests and 58.7% knew that it can interfere with cardiac markers, only 7% knew it could interfere with pregnancy or vitamin D tests, less than 3% knew that it could interfere with HIV and hepatitis testing, and a whopping 19.5% were convinced biotin didn’t interfere with any testing at all. Since the sample was enriched in biotin-prescribing dermatologists, it probably overestimates the knowledge of this issue among physicians more broadly.
Thus, physician knowledge of this issue is very inadequate, and most patients are likely to be totally unaware of it.
Now let’s dig into the nature of the problem, its scope, how bad it is, and what we can do about it.
How Biotin Generates False Measures on Lab Tests
The reason that high doses of biotin can generate false measures on lab tests is that many lab tests use biotin as part of their internal machinery to test the level of other things in the blood or urine. Since high-dose biotin supplements cause a much greater than normal level of biotin and its breakdown products to appear in the blood and urine, this can mess with the internal machinery of the test.
Specifically, this is a problem with biotin-based immunoassays. Immunoassays rely on antibodies to detect many other types of molecules. Compared to other methods, such as liquid chromatography, immunoassays are more likely to have problems with accuracy, precision, and interference. However, they are extremely common because they are well suited to run large volumes of samples per unit of time with minimal technical skill required from lab personnel. Since personnel are the most expensive input into the costs of lab tests, using immunoassays saves a lot of money.
Most immunoassays use biotin as part of their internal machinery. For example, a 2018 paper by the Canadian company Calgary Laboratory Services reported that “we are a relatively large laboratory with an annual volume of 25 million chemistry tests” and that “most of our immunoassays are vulnerable to biotin interferences.”
The reason biotin is used in these assays is to exploit the principle of the tight binding between biotin and a group of structurally related proteins known as avidin or streptavidin.
The origin of this principle is found in early experiments of the 1920s and 1930s leading to the phenomenon known as “egg white injury.” In the budding field of nutrition science, early findings suggested that egg whites could not provide adequate protein for the growth of rats. However, a paradox emerged showing that small amounts of egg white did allow for maximal growth, while large amounts did not. This suggested there was something toxic in egg white. Eventually, it was discovered that egg whites contain a protein now known as avidin, which binds biotin and prevents its absorption from food. Thus, large amounts of egg white were causing biotin deficiency.
Subsequently, in the 1950s scientists realized they could use avidin as an experimental tool. Since it bound tightly to biotin, they could use it to purify biotin and biotin-bound enzymes, and to study where those things went when they moved around inside cells. Then, in 1980, scientists published the first method to expand its use into immunoassays to measure all kinds of things.
It turns out that there are likely over 100 avidin-like proteins, and they are found not only in the eggs of birds, amphibians, and reptiles, but are also made by fungi and bacteria. The form made by the bacterium Streptomyces avidinii is known as streptavidin. The many different versions of avidin are called homologs. Since the bacterial forms are most often used in modern immunoassays, the whole group of homologs is often referred to in the scientific literature collectively as “streptavidin.”
The bond between streptavidin and biotin has several properties that make it ideally suited to use in immunoassays:
The bond is very specific. Apart from biotin and its derivatives, streptavidin binds very little else.
Chemical bonds can be broadly categorized into covalent bonds, where if two things join they become a single molecule, and non-covalent bonds, where two things can join while maintaining their own chemical identity. The bond between streptavidin and biotin is the strongest non-covalent bond between a protein and another molecule ever identified.
The bond is very resistant to changes in pH and to chemicals used in lab assays that tend to break many other bonds.
Since biotin is a very small molecule, it can link things together within the assay without obstructing other processes that need to happen to complete the measurement.
Soon after their development in 1980, biotin-based immunoassays became very common. The first case of biotin interference was reported in 1996. An infant was proactively given 10 milligrams of biotin along with 20 milligrams of thiamin and 10 milligrams of riboflavin because her sibling had died of an unknown metabolic disorder two years earlier. This caused her TSH to appear falsely low and her free T4 falsely high in routine screening.
The FDA first issued guidance about biotin interference with lab tests in November of 2017, 21 years later, and has reiterated the guidance numerous times since. The first issuance was in the year following the receipt of a reported death. A multiple sclerosis patient had been taking high-dose biotin. After an acute episode of apparent heart attack, the patient had low cardiac markers that may have been falsely low as a result of biotin interference. If this is correct, it may have played a role in improper treatment decisions that led to patient’s death. However, there was too little information for the FDA to agree with the report. Nevertheless, reports of interference with cardiac markers kept coming in, leading the FDA to finally issue guidance.
Since the FDA guidance, research into this issue has proliferated and we can now appreciate how large the scope of the problem is.
There are two main types of biotin-based immunoassays: sandwich assays, where high-dose biotin causes false decreases in the measurement, and competitive assays, where high-dose biotin causes false increases in the measurement.
How Biotin Causes False Decreases in Sandwich Immunoassays
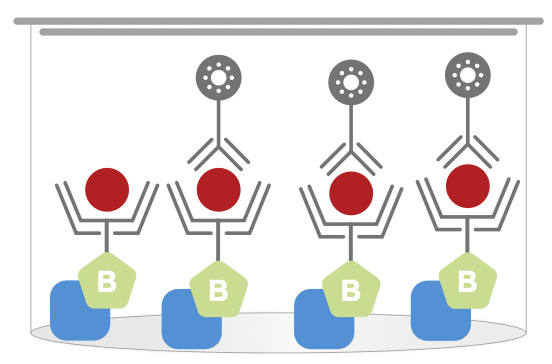
Borrowing from Figure 1 in this paper, biotin-based sandwich immmunoassays have four main components:
The analyte is whatever you are trying to measure in the sample.
The labeled antibody is what your machine can actually measure. In most cases, the labeled antibody will give off light, and a machine called a spectrophotometer will measure how much light is given off. However, it could be labeled in a different way, such as with radioactivity. I will assume light-based, or luminescent, antibodies are used for the rest of this description.
In order to make a successful measurement, you want the labeled antibody — and therefore the amount of light emitted from the sample — to be proportional to the analyte. That requires having more labeled antibody than needed to bind to all of the analyte, as well as a way to get rid of any excess of labeled antibody. That is where the other two components come in.
The biotinylated antibody will bind to the other side of the analyte and anchor it to the floor of the measuring container, which is lined with streptavidin-coated microparticles. Usually this container is a “microplate,” which has many small wells for measuring many samples at once, though it could be a tube or something else. I will assume microplates, or “plates,” are used for the rest of this description.
If you mix all these components together, all of the analyte will get “sandwiched” between the two antibodies, bound to the streptavidin-coated microparticles lining the plate, with the luminescent antibodies sticking out on top. At this point, you wash away the remainder of the luminescent antibodies, and the amount of light emitted from the plate is exactly proportional to the amount of analyte present in the sample.
It looks like this:
This diagram, of course, is simplified to make this easier to visualize. In reality, there there are far more than four binding sites in each plate well.
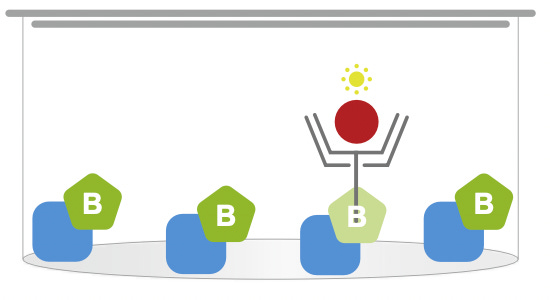
The problem is that if there are very high concentrations of biotin in the sample because the person was taking high-dose supplements, the biotin itself will bind to the streptavidin-coated microparticles, displacing the biotinylated antibodies, thereby taking up spaces needed for the “sandwiched” analyte, causing it to be washed away during the wash step rather than bound to the bottom of the plate.
It will look like this, where each green B represents a molecule of biotin from the sample:
Thus, high-dose biotin supplements cause false decreases in sandwich assays.
How Biotin Causes False Increases in Competitive Immunoassays
Borrowing from the same figure, these are the main components of a biotin-based competitive immunoassay:
Everything is the same, except the labeled antibody has been replaced by a labeled analyte.
The principle that the analyte will be bound to the biotinylated antibody, which will anchor it to streptavidin-coated microparticles lining the bottom of the plate is the same.
However, rather than being sandwiched by a biotinylated antibody, the analyte competes with a luminescent form of itself provided in the assay kit, referred to here as the labeled analyte.
In this case, if the concentration of the analyte in the sample were zero, all of the binding sites on the biotinylated antibody would be bound by the luminescent analyte from the kit, and the spectrophotometer would read a high signal. The more analyte there is in the sample, however, the more it competes for binding to the biotinylated antibody, making the signal decrease.
It will look like this:
Since there were two molecules of analyte in the sample, they displaced two of the four labeled analyte molecules, and cut the signal in half.
However, if there are high concentrations of biotin in the sample, it will displace the biotinylated antibodies, decreasing the signal without any need for the analyte to be present:
Here there is no analyte at all, yet because there is a lot of biotin in the sample the biotin takes up three out of four binding sites. This causes a 75% decrease in the signal as if there were a high analyte concentration, even though there is no analyte in the sample at all.
Thus, high-dose biotin supplements cause false increases in sandwich assays.
Overall, the role of high-dose biotin in both cases is to displace the binding of biotinylated antibodies to the streptavidin-coated microparticles and to decrease the amount of luminescence measured by the spectrophotometer. However, whether this causes a false decrease or a false increase depends on whether the principle of the assay involves the luminescence increasing or decreasing with the analyte concentration. In sandwich assays, the luminescence increases as the analyte concentration increases, so biotin causes a false decrease in the measurement. In competitive assays, the luminescence decreases as the analyte concentration increases, so biotin causes a false increase in the measurement.
There are a great many biotin-based immunoassays that may introduce many variations to this theme, but what I have presented above is a general scheme for understanding how biotin interference typically works.
Which Lab Tests Are Potentially Impacted by High-Dose Biotin Supplements?
A recent comprehensive review of this issue characterized the scope of the problem.
Whether an assay is biotin-based and how sensitive it is depends on the assay design.
Manufacturers of biotin-based assays measure the threshold needed for biotin interference and compare it to the blood values of people taking supplements. There are limitations to this approach, but it casts the broadest net.
Among common autoanalyzers used by medical laboratories, the platforms made by Roche Diagnostics have 81 assays susceptible to biotin interference, 44 of which are “very susceptible.” The platform made by Ortho Clinical Diagnostics has 30 susceptible assays, 28 of which are “very susceptible.” The platforms made by Siemens have 21 susceptible assays, 6 of which are “very susceptible.” The platforms made by Beckman Coulter have 15 susceptible assays, 6 of which are “very susceptible.”
Among the most commonly reported interferences in the literature are the following:
Thyroid Function: False decreases in TSH and thyroglobulin; false increases in free and total T4, free and total T3, and anti-thyroid antibodies. This could lead to a false diagnosis of hyperthyroidism, the masking of hypothyroidism, or a false diagnosis of an autoimmune condition.
Other Hormones: False decreases in parathyroid hormone (PTH), luteinizing hormone (LH), follicle-stimulating hormone (FSH), growth hormone, insulin, C-peptide, adrenocorticotropic hormone (ACTH). False increases in testosterone, DHEA-sulfate, estradiol, progesterone, and cortisol. This could lead to a false diagnosis of hypoparathyroid hormone, wrong suspicion a pituitary problem, or wrong suspicion of a hormone-secreting tumor.
Cardiac Markers: False decreases in troponin and creatine kinase-MB, the form of creatine kinase abundant in heart muscle; and NT-proBNP, a marker of heart failure. False increases in digoxin, a medication used for heart problems. This can lead to masking of a recent heart attack, a recent case of heart failure, or a mistake in dosing medication.
Viral Serology: False positives for HIV and markers for hepatitis A, B, and C.
Tumor Markers: False increases of alpha-fetoprotein, cancer antigen 125, carbohydrate antigen 19-9, and free and total prostate specific antigen (PSA).
Vitamin Markers: False increases in vitamin D, B12, and folate.
Pregnancy: Invalid results or false negatives on home pregnancy tests in women who are pregnant.
Allergies: False negatives for IgE allergies regardless of the allergen, including in patients with anaphylaxis.
Studies Simulating High-Dose Biotin Supplementation In Vitro
Not all of these tests are equally susceptible.
One way to compare them is to look at how they perform when biotin is added to the sample in the laboratory. To do this, researchers use existing estimates of what blood levels of biotin reach on different supplement doses and then spike the samples with these concentrations. This simulates biotin supplementation in a way that can be used to easily and quickly test the performance of many different assays.
One paper looked at the performance of over 30 different assays on a Roche Elecsys autoanalyzer platform. Normal concentrations of biotin in plasma are less than 1 nanogram per milliliter (ng/mL). They spiked samples with biotin to bring them to 15.6 ng/mL to simulate patients supplementing with 5 milligrams biotin per day (mg/d); to 31.3 ng/mL to simulate 10 mg/d; and to 500 ng/mL to simulate the peak concentration reached after a dose of 100 milligrams, or what might be seen randomly throughout the day in someone taking 300 mg/d.
With the simulation of 5 mg/d, most assays performed with minimal bias. However, the thyroid marker TSH and the cardiac marker troponin T were falsely decreased by 10%. Various anti-thyroid antibodies were falsely increased by 10%.
With the simulation of 10 mg/d, the false increase for anti-thyroid antibodies increased to 50% for anti-thyroglobulin and more than 2-fold for antibodies against thyroid peroxidase (anti-TPO) and the TSH receptor (anti-TSHR). The false decrease for TSH reached 25%; for troponin T it reached 20%; luteinizing hormone (LH), follicle-stimulating hormone (FSH), testosterone, DHEA-sulfate, and folate emerged with 10% false decreases. These last three were paradoxical, because models of how the assay works suggest they should be falsely increased rather than falsely decreased, as is found at higher concentrations.
It was with the simulation of 100-300 mg/d where things really fell apart. TSH, FSH, insulin, pro-BNP, troponin T, free and total PSA, PTH, and ACTH all had 90-95% false decreases. Folate and cortisol were falsely increased almost 2-fold; vitamin B12, progesterone, DHEA-sulfate, and estradiol were falsely increased between 2- and 4-fold; testosterone and free T4 were falsely increased between 4- and 8-fold; the medication digoxin was falsely increased 15-fold; and the anti-thyroid antibodies were falsely increased between 20- and 60-fold.
Another paper used a similar approach to evaluate the performance of the Vitros 5600 autoanalyzer platform produced by Ortho Clinical Diagnostics. They spiked samples to yield eight different concentrations of biotin between 1.56 and 200 ng/mL. They only tested seven different assays. Troponin I and hepatitis antibodies were stable. TSH and prolactin were the most sensitive, suffering false decreases even at low concentrations. Cardiac creatine kinase, cortisol, the tumor marker alpha-fetoprotein, ferritin, and the pregnancy marker beta-hCG all required 12.5 ng/mL biotin to see some effect. At 50-200 ng/mL biotin, most tests were profoundly affected: cortisol was doubled, cardiac creatine kinase and TSH were brought close to zero, ferritin was cut by 10.4-61.5%, alpha-fetoprotein and prolactin were cut up to to 90%, and beta-hCG was falsely decreased 65-94%.
This suggests that doses in the 100 mg/d range are likely to cause serious errors, including false negatives on pregnancy tests.
A paper published earlier this year looked for the first time systematically at allergy tests. Spiking samples from known allergy patients to 300-1200 ng/mL biotin — achievable in the hours after acute doses in the 100 mg range — could render false negatives for any IgE allergy tested (cashew, bee stings, peanuts), even in anaphylactic patients.
While these systematic in vitro tests are very important for rapidly characterizing the scope of the assays impacted, they are likely to be gross underestimates of the problem.
In Vitro Tests Underestimate Biotin Interference
There are several reasons in vitro tests underestimate the biotin interference problem:
In a live human being, a large portion of biotin breakdown products — called “metabolites” — are present in the blood and urine alongside biotin. Some of them also bind to streptavidin. Thus, it is the concentration of biotin and all its streptavidin-binding breakdown products, not merely of biotin itself, that will determine the level of interference.
Large molecules bound to biotin will also bind to streptavidin. These have been traditionally filtered out of samples when measuring biotin in the samples for this reason. However, they are not filtered out of samples for routine lab tests using biotin-based assays.
People with kidney problems, and perhaps other illnesses such as impaired liver function, will accumulate more biotin in their blood than normal, and thus have a greater degree of interference on lab tests.
After an acute dose of biotin in the 0.5-20 milligram range, 45% of the biotin excreted in the urine is biotin metabolites. In plasma, 25-40% of a 1200-microgram dose is biotin metabolites, and this stays stable after two weeks of taking the supplement daily.
While biotin metabolites have strong competition with biotin for binding to egg white avidin, their binding to the streptavidin used in most modern immunoassays is less significant. Some of them have no appreciable binding to streptavidin, and the others bind about 10% as strongly. This suggests that in vivo results should show small rather than large differences for biotin interference when compared to in vitro results. However, streptavidin binds unknown interfering substances in human urine that egg white avidin does not. If we do not know all the streptavidin-binding substances in human samples, this makes strongly underscores the importance of conducting biotin interference studies in live humans.
Another problem is that individuals with impaired kidney function may accumulate much more biotin and biotin metabolites than those with normal kidney function.
Remarkably, a pubmed search for biotin and chronic kidney disease (CKD) reveals only a single human study showing massively high vitamin B12 levels in CKD patients. The authors suspected biotin interference, but they “ruled out” biotin therapy based on “a thorough patient history.” Bizarrely, they did not measure the serum levels of biotin.
It is also possible that impaired kidney function alters the distribution of metabolites or leads to the accumulation of biotin-bound proteins that are capable of binding streptavidin. This is supported by a case of falsely low PTH in a kidney disease patient. The patient was supplementing with 10 milligrams of biotin per day. Her PTH was high, but falsely measured low. The authors measured the biotin in her blood, and it was 4.8 ng/mL, which is high. However, the assay manual said this concentration of biotin was insufficient to create interference. Moreover, when they spiked a control sample with that concentration of biotin, it did not create any interference. However, removing the “biotin” from her blood using streptavidin removed the false PTH suppression in her sample. When she stopped the supplement for two weeks, this also removed the false PTH suppression in her sample. Therefore, the 10 milligram per day biotin supplement was causing something other than free biotin to accumulate in her blood that was capable of binding streptavidin and was causing interference in the assay.
Searches for liver disease and serum biotin do not reveal anything looking at whether liver disease can alter serum biotin levels, but there is evidence from rats that the liver has a biotin storage system. So perhaps liver damage can also raise serum biotin.
The Mayo Clinic study cited at the beginning of this article measured biotin levels in 1,442 blood samples leftover from electrolyte measurements in the emergency room. Unfortunately their assay had a limit of detection of 5 ng/mL, which is more than five times the top of the normal range. 48% of the samples had biotin concentrations higher than this. It is not normally possible to have biotin concentrations this high without high-dose supplements. Yet their outpatient survey revealed only 7.7% of respondents taking high-dose supplements, which is consistent with the number of women over 60 taking such supplements nationally. Unless biotin is putting people in the emergency room in droves, or unless people with emergency medical problems are typically reaching for the high-dose biotin on their way to the ER, I would think illness — at least from kidney impairment, and perhaps from liver damage or other mechanisms — is driving serum biotin upward.
CDC estimates that chronic kidney disease impacts 14% of Americans. Nonalcoholic fatty liver disease impacts 20-30% of individuals in Western countries.
Thus, biotin interference in live humans is likely to be worse than the in vitro simulations suggest because of the presence of biotin metabolites and biotin-bound proteins in human samples, and because people with kidney disease or perhaps other illnesses are likely to have greater than expected accumulation of these substances and possibly an altered distribution of them as well.
In Vivo Studies of Biotin Interference in Lab Tests
A small study of six individuals measured 37 assays for 11 analytes across four platforms before and after taking 10 milligrams of biotin a day for seven days, and after stopping the supplement for another seven days. This was a before-and-after study rather than a randomized controlled study. They didn’t compare the biotin-based tests to other tests not based on biotin, so there is some possibility that there was a real effect of biotin. However, the results are consistent with what we know about biotin causing false alterations on these tests, and it is the only systematic investigation of many assays in live humans supplementing with biotin, so we need to take a look at it.
The supplement decreased TSH by 1.67 mIU/L on the Vitros platform, but only by 0.72 mIU/L on the Roche platform.
PTH was decreased by 25.8 pg/mL on the Vitros platform, which is nearly half the reference range.
25(OH)D went up 9.25 ng/mL on the Roche platform, which is enough to misclassify many people with suboptimal status as having optimal status.
Thyroid hormones were fairly stable, but on the Roche platform total T3 increased above the reference range in half the subjects.
Let’s compare this paper where humans took 10 mg/d to the in vitro simulations of 10 mg/d cited above:
For Roche TSH, the simulation found a 25% decrease, while the human study found a 67% decrease. Thus, the simulation underestimated the effect by 2.7-fold.
For Vitros TSH, the simulation found an 87-96% decrease, while the human study found a 96% decrease. Thus, the simulation was fairly accurate.
These are the only two examples where we can clearly line up the studies. It is sufficient to illustrate the point that the in vitro simulations can sometimes but not always be gross underestimations of the interference found in vivo.
Unnecessary Medications and Surgeries, Misdiagnoses, and Psychological Distress
To see the clinical impact of this problem, as well as the realistic worst-case scenarios, we now turn to the case reports.
Unnecessary Antithyroid Medication
In a series of six children taking between 2 and 15 milligrams of biotin per day for inherited metabolic diseases, all six were found to have apparent Graves’ disease during routine labwork. They had high thyroid hormone levels, low TSH, and high levels of anti-TSH receptor antibodies. Only one child had symptoms consistent with hyperthyroidism (tachycardia, restlessness, failure to thrive). Given that he had a metabolic disorder, these symptoms are not specific to his thyroid. At least three of the children were started on antithyroid medication. All of the abnormal bloodwork normalized after stopping the biotin supplements for one to seven days. The antithyroid medication may have harmed the children who took it, but this possibility was not pursued in detail.
A similar case is found in a 32-year-old man. His general practitioner found low TSH and elevated thyroid hormones, and referred him to an endocrinologist. The endo found no clinical signs of hyperthyroidism. However, “positive” antibodies to the TSH receptor “confirmed” Graves’ disease, and the patient was given antithyroid medication. When it was time for followup, his endo was on vacation so he was referred to a hospital. Surprised by his “‘frank and severe’ biochemical hyperthyroidism” despite “no signs of thyrotoxicosis,” the hospital physicians noticed all his bloodwork had been done at the same lab so they repeated it in-house, where they used a different platform. All the results turned out to be normal.
It turned out he had been taking 300 milligrams of biotin per day as part of a clinical trial for X-linked adrenomyeloneuropathy.
His unnecessary antithyroid medication was then stopped immediately.
The authors chose a somewhat bizarre title, “A Somewhat Bizarre Case of Graves Disease Due to Vitamin Treatment.”
Rather, the patient did not have Graves’ disease at all.
Unnecessary Surgery
In a 15-year-old girl with Denys-Drash Syndrome, biotin interference led to unnecessary removal of her ovaries. This is a disorder involving impaired kidney function and, usually in males, abnormal sexual development. In this case, the girl did have abnormally developed sexual organs. She had high testosterone. Based on previous cases the physicians worried she had a testosterone-producing tumor, so they removed her ovaries. However, no such tumor was found during the removal. Her testosterone remained high, at which point further questioning revealed she had been been taking high-dose biotin for eight months for hair loss. Her testosterone was then remeasured using liquid chromatography and shown to be normal, and the original immunoassays also showed her testosterone to be normal after she stopped taking biotin.
They do not report the dose of biotin she was taking, but her serum biotin levels were 800 milligrams per liter, which is 800 micrograms per milliliter, and 800,000 ng/mL. This is orders of magnitude higher than what would be expected from 100-300 milligrams per day, and may be a calculation error or an error in reporting the units. However, it may also be supportive of her kidney impairment backing up her biotin clearance.
Had the false testosterone measurement been discovered prior the surgery, she would not have had the surgery.
Psychological Distress, Near Unnecessary Surgery
A 48-year-old woman came to an endocrinology clinic with heart palpitations, difficulty losing weight, and hirsutism, which is hair growth in a typically male pattern.
She had been taking 5 milligrams of biotin per day regularly for six months, and intermittently for five years.
She had a multitude of aberrant hormone measures that led to an MRI of her pituitary gland to look for a tumor. Then she was referred to the reproductive endocrinology unit to look for a testosterone-producing tumor or an ovarian hyperthecosis, which is an overgrowth of part of the ovaries. Her pelvic ultrasound was unremarkable, but could not rule out a small testosterone-producing tumor.
Therefore, she was scheduled for a hysterectomy and oophorectomy, which are the surgical removals of the uterus and ovaries.
Luckily, ten weeks after her initial presentation and before her scheduled surgery, additional results using liquid chromatography rather than immunoassay showed all her hormone levels were normal. The patient stopped taking biotin, and then repeated the immunoassays two weeks later, and they too were normal.
This led to weeks of psychological distress and almost resulted in an unnecessary surgery.
Interestingly, a 2017 report of a different case of falsely elevated sex hormones actually did result in a totally unnecessary hysterectomy and bilateral oophorectomy, and the source of the false elevations was never identified. All that was shown was that the clinical picture contrasted with the results of the immunoassays, and liquid chromatography results showed the immunoassays were wrong. The authors ruled out biotin interference because “our patient did not use biotin at the time of testing,” but they did not measure her serum biotin.
I believe not measuring serum biotin is a gross error in these cases regardless of whether the patient reports using biotin. Patients do not always remember what they are taking, they do not always know the ingredients of multivitamins or dermatological supplements they are taking, and there may be other reasons besides supplements for a raised serum biotin.
Confusion Around Necessary Surgeries
In two women in their 60s, PTH was rendered undetectable from biotin interference.
The first woman was suffering from primary hyperparathyroidism that was causing high serum calcium, osteopenia, fractures, and chronic kidney impairment. Her problem was her PTH was too high. Yet, as she was preparing to have it surgically removed, her PTH became undetectable. This made no sense, because her serum calcium was high, and PTH raises serum calcium. It turned out she was taking 1500 micrograms per day of biotin for hair growth. She stopped the biotin, and her PTH was repeated a month later. It was normal. To make the biotin interference clear, she restarted the same dose, measured the PTH again, and it disappeared.
While 1500 micrograms is way too low to do this according to the studies I reviewed above, this patient’s elevated PTH was causing chronic kidney impairment. Thus, her serum biotin was probably much higher than you would expect from her supplement, and she may have had an altered distribution of biotin metabolites or biotin-bound proteins. Once again, however, serum biotin was not measured.
In the second case, the woman had elevated PTH causing elevated serum calcium and kidney stones for ten years, and more recently she was suffering from muscle pain. Her parathyroid gland was partly removed, and her PTH and calcium returned to normal. At 6 and 9 months out, however, her PTH became undetectable, most likely because she was taking 5 milligrams of biotin per day for neuropathic pain.
This is not a comprehensive review of case reports and case series. Rather, I selected specific cases that help illustrate some of the clinical harm that comes from biotin interference.
What Can Be Done About Biotin Interference?
Up to this point, laboratorians have had various ways to look for and correct for interference. For example, if results are anomalous, they can perform a serial dilution. This yields a string of repeated dilutions such as 2x, 4x, 8x, 16x, and so on. This should yield analyte concentrations that are proportional to the degree of dilution. If it does not, this is a sign of interference. Sometimes, simply diluting the sample will bring the interfering factor — in this case biotin — down to low enough concentrations that the assay performs normally.
If biotin interference is suspected, there are several other options:
Remove biotin from the sample using streptavidin-coated microparticles before making the measurement.
Use liquid chromatography to repeat the measurement rather than immunoassay.
Alert the physician and patient, and retest after the patient stops taking biotin.
However, all of these techniques are very time-consuming, and liquid chromatography is more expensive than immunoassay.
Thus, lab manufacturers and methodologists have been working hard for the last several years to make immunoassays “immune” to this problem.
One innovation published this year is a synthetic “mirror image” streptavidin. Many molecules are capable of a phenomenon known as optical isomerism. They can exist in two mirror image forms, each of which rotate light in opposite directions. The mirror images that rotate light leftward are designated L for levorotatory and those that rotate light rightward are designated D for dextrorotatory. This is true of both streptavidin and biotin. Natural streptavidin is a protein made of L-amino acids, and natural biotin is D-biotin. D-biotin is also the form found in high-dose supplements. Scientists have now made a synthetic streptavidin composed of D-amino acids that binds tightly to synthetic L-biotin. Since D-streptavidin will not bind to D-biotin, supplementation with D-biotin will not be able to cause interference.
Another method was published this year to increase the number of streptavidin microparticles per sample in a fully automated platform. This pushes up the number of binding sites so that it becomes irrelevant whether large amounts of biotin compete for them. While this may seem obvious in retrospect, the microparticles themselves can block the light signal and too high a concentration can interfere with the assay. Thus, work had to be done in designing microparticles that could be added in higher concentrations without blocking too much of the signal.
Nevertheless, while lab assays will likely have this problem solved in the future, right now physicians and patients have no control over the degree to which the problem is solved, nor any control over the skill of the lab technicians in recognizing biotin interference.
Therefore, physicians need to ask their patients about biotin intake, remind them to stop taking biotin before any lab tests, and be aware of biotin interference as a reason for anomalous lab results that conflict with the clinical picture.
Individuals have no control over their doctor’s knowledge in this area, and need to take the initiative to stop taking biotin before any lab tests.
But for how long do we need to stop taking biotin?
How Long to Stop Taking Biotin Before Lab Tests
Lab manufacturers make claims in their documentation about the threshold of serum biotin needed to cause interference, and often this threshold is 10 ng/mL or higher.
However, we saw above that humans taking 10 milligrams per day have 2.7-fold greater false suppression of TSH on the Roche assay than is found when simulating that intake in vitro.
We also saw that a woman taking as little as 1.5 milligrams per day has falsely undetectable PTH. Unfortunately, we do not know her serum biotin and it was likely higher than we would expect from that dose due to impaired kidney function.
We also saw that another patient with kidney disease taking 10 milligrams was generating something other than free biotin in her blood that was causing false suppression of PTH.
Therefore, we should not put all of our eggs in the basket of seeing how long it would take to allow serum biotin to fall into the range that the lab manufacturer says is OK.
Rather, we should look at how long it takes to clear serum levels to what we would find in those not taking any supplement, and especially at how long it takes to clear actual interference with lab tests.
A single dose of 600 micrograms of biotin caused a the serum biotin to rise from 0.75 ng/mL to a max of around 3.25 ng/mL at one hour. It was cleared from plasma with a half life of 1 hour and 50 minutes. Generally 94-97% of something is cleared after 4-5 half-lives. Thus, a single 600-microgram dose should be gone from plasma in 9 hours.
From the same study, a week of taking 300 micrograms every day raised the fasting level from 0.75 to 0.94 ng/mL, and another week of 600 micrograms per day raised it to 1.25 ng/mL. The fact that the fasting serum level is increasing after repeated daily dosing shows that even after 24 hours the biotin is not being fully cleared from plasma. It may be that the half-life is rising with cumulative dosing, or that the fasting level represents a natural floor in the circulating biotin that is proportional to body stores, and that body stores were increasing throughout the study.
While this study was short, it provides proof of principle that it takes longer for plasma levels to return to baseline when the supplement is taken regularly over time.
Doses in the 100-300 milligram range have extended plasma half-lives, and taking the biotin with food instead of fasting delays the absorption and extends the plasma half-life. Overall these high doses have plasma half-lives between 7.8. and 18.8 hours. This suggests it would take 1.5-3.9 days to clear most of the dose from plasma. Rounding up, four days should be sufficient.
There is no data available on how long it takes to clear the biotin levels reached after months of supplementing with these high doses, or with months of supplementing with intermediate doses in the 1-10 milligram range.
However, we do have some data on how long it takes to remove interference on lab tests after stopping biotin:
In the original case report of an infant with falsely low TSH and falsely high T4, these values appeared to normalize after 2 days of stopping biotin.
One author caring for an infant on 30 milligrams of biotin per day with apparently altered thyroid tests performed an experiment on himself by ingesting a single dose of 30 milligrams of biotin. The report claims that many interferences lasted for approximately five hours while thyroid markers “endured for up to 24 hours.” However, the thyroid markers are shown in Figure 1 and although they are largely recovered, they are not fully recovered at 24 hours.
In a group of ten healthy adults, taking 5 milligrams biotin per day for seven days mainly altered thyroid markers for two hours after cessation. However, TSH and anti-TSH receptor antibodies took a full day to recover. The antibodies were the most affected.
In a study of lab interferences caused by high-dose biotin in multiple sclerosis patients, two of the study authors performed a side-study on themselves and took 15-30 milligrams of biotin per day for three days. Interferences with hormone and vitamin D measurements cleared within 48 hours.
In the six children misdiagnosed with Graves’ disease, stopping the 2-15 milligrams per day of biotin that had apparently been taken for months or years took 24-48 hours to clear the interference with TSH and thyroid hormones, but took up to seven days to clear the effect on anti-TSH receptor antibodies. These authors did not show all of the data, but they appear to have performed daily tests throughout the first week.
Other studies and case reports showed return to normal levels after one or two weeks, or after one month, without testing other time points.
I am not aware of any studies showing that it takes longer than one week to remove any interference.
There are two interpretive problems here:
We have no data on how long it takes to clear biotin from plasma when one has spent months or years on a given dose.
It may be the case that ill people, especially those with kidney disease, take longer to clear biotin.
It is notable that in the study of ten healthy adults, anti-TSH receptor antibodies were the most impacted by interference, and along with TSH took the longest to recover, but only took 24 hours. In the six children taking 2-15 milligrams of biotin per day for very long periods of time, anti-TSH receptor antibodies took the longest to recover, but in their case this meant seven days. Both of these studies are consistent with the Roche in vitro simulation showing that the anti-TSH receptor antibody test is the most vulnerable to biotin interference, although in that study the other thyroid antibodies were very close behind.
Did the children require seven days to clear their false positivity on that test because they were children? Or because they had metabolic disorders? Or because they had likely been taking the biotin for years?
A few things are clear:
The worst thing you can possibly do is take a high-dose biotin supplement the morning of your lab test.
In most cases, most of the problems will be gone with one day, but very high doses take four days to clear, and many tests take 48 hours to clear in some people.
Some tests will take some people up to a week off of biotin to clear. Presumably this is driven by a combination of the vulnerability of the specific test, the health of the person taking the biotin, and the length of time for which the person has been taking biotin.
My suggestion would be to stop any biotin supplements over 1 milligram per day for at least two days and preferably four days before any lab testing.
Wait a full seven days before running thyroid-related antibodies if any of the you have impaired kidney function or if you have been taking the supplement consistently for months or years.
If you have been using high-dose biotin supplements, don’t make any major medical decisions without making sure lab work they are based on was repeated with liquid chromatography rather than immunoassay.
The Bottom Line
Doses of biotin greater than one milligram per day can interfere with dozens of different lab tests.
There are reasons to believe that interference is worse in live humans than suggested by test tube studies and by the assay manuals published by lab manufacturers. There are not enough human supplementation studies to clarify how long interference lasts using different doses of biotin for different durations in different contexts. Therefore, we should err on the side of caution.
The worst thing you can ever, ever do regarding this issue is to take biotin the morning of a lab test. Never, ever do this.
While many lab tests will normalize hours after taking a biotin supplement for many people, many will take 24-48 hours, and some tests will take some people up to seven days. The tests that appear to be impacted the most are thyroid-related antibodies.
Therefore, we should approach this as follows:
Never take any biotin supplement before a lab test on the same day as the test.
Always stop taking biotin supplements that have doses larger than 1 milligram for at least two days and preferably four days before any lab tests.
Before measuring thyroid-related antibodies, cut out the supplement for a full week if you have been taking it for months or years or if you have impaired kidney function.
If you wish to exercise an abundance of caution, there is nothing wrong with cutting out the biotin for a full week before lab tests.
Physicians should always ask their patients about biotin supplementation, advise them to stop biotin for at least 2-4 days before lab tests, and be aware of biotin interference as an explanation for anomalous results.
If you have been taking biotin in doses higher than one milligram per day, even if you have followed the above, do not make any major medical decisions without either repeating immunoassay tests with liquid chromatography to confirm their accuracy or cutting out the biotin supplement for one months to confirm the results are repeatable.
With all this said, how necessary are these high doses?
In High Protein? You Need More Biotin, I made the case that many people need 150-300 micrograms per day, depending on how much protein they eat. My simple food-based recommendations for getting enough biotin are found in my Cliff Notes (free for Masterpass members here).
Certainly milligram doses are needed for genetic metabolic disorders in biotin absorption and utilization. But do most people taking high-dose supplements need them?
That will be the topic of the next article. Make sure you are subscribed, so that you get notified as soon as that article comes out.
Disclaimer
I am not a medical doctor and this is not medical advice. My goal is to empower you with information. Please make all health decisions yourself, consulting sources you trust, including a caring health care professional.
Stay Immune Through the Winter
My new 7-page quick guide on how to not get sick this winter, Staying Immune Through the Winter, is free for everyone. All you need is a free or paid subscription to my Substack.
If the box above says “subscribed,” this means you are a Masterpass member and can download the guide here.
If the box says “upgrade to paid,” then you are a free subscriber and your guide is currently sitting in your inbox. Search your mail, spam, and trash for “staying immune through the winter” and make sure anything from Substack is going to primary.
If it allows you to enter your email address, do so, hit “subscribe,” and then find the email from “Chris Masterjohn, PhD” with the subject “Welcome to My Newsletter!” If you can’t find this, try searching for either of those terms and for “Substack.” At the top of the welcome email you will find your downloadable guide to not getting sick.
Join the Next Live Q&A
Have a question for me? Ask it at the next Q&A! Learn more here.
Join the Masterpass
Masterpass members get access to premium content (preview the premium posts here), all my ebook guides for free (see the collection of ebook guides here), monthly live Q&A sessions (see when the next session is here), all my courses for free (see the collection here), and exclusive access to massive discounts (see the specific discounts available by clicking here). Upgrade your subscription to include Masterpass membership with this button:
Learn more about the Masterpass here.
Please Show this Post Some Love
Please like and share this post on the Substack web site. This will help spread it far and wide, as subscriber likes drive the Substack algorithm. Likes from paid subscribers count the most, but likes from free subscribers come in the highest numbers and are the foundation for spreading the content.
Take a Look at the Store
At no extra cost to you, please consider buying products from one of my popular affiliates using these links: Paleovalley, Magic Spoon breakfast cereal, LMNT, Seeking Health, Ancestral Supplements, MASA chips. Find more affiliates here.
For $2.99, you can purchase The Vitamins and Minerals 101 Cliff Notes, a bullet point summary of all the most important things I’ve learned in over 15 years of studying nutrition science.
For $10, you can purchase The Food and Supplement Guide for the Coronavirus, my protocol for prevention and for what to do if you get sick.
For $10, you can purchase Healing From COVID Vaccine Side Effects for yourself or a loved one if dealing with this issue. It also contains an extensive well-referenced scientific review, so you can also use this just to learn more about my research into the COVID vaccines.
For $15, you can pre-order a single format of my Vitamins and Minerals 101 book, my complete guide to nutrition, which I am currently working full-time on finishing.
For $25, you can pre-order a digital bundle of my Vitamins and Minerals 101 book.
For $29.99, you can purchase a copy of my ebook, Testing Nutritional Status: The Ultimate Cheat Sheet, my complete system for managing your nutritional status using dietary analysis, a survey of just under 200 signs and symptoms, and a comprehensive guide to proper interpretation of labwork.
For $35, you can pre-order a complete bundle of my Vitamins and Minerals 101 book.
For $250-$1499.99, you can work one-on-one with me.






Great and informative article! I had only heard about the TSH test interference. But this is great to know for any future labs. The case of the girl having the surgery is tragic. Look at the dangerous conclusions people can jump to without sufficient knowledge and context of the individual's nutrition.
Also if you made a video on this, I bet it would get a lot of hits. I think on Youtube a lot of vloggers talk about biotin for the skin/hair benefits. But I'm certain they don't know about all these possible effects on their labs that could cause distress. "Taking biotin? Watch out for this!" Thumbnail is someone with nice hair but with a very panicked look on their face, haha.
Thank you! Good info. I’ve taken 10,000mcg daily for 10 yrs for thinning hair. It does seem to help. My ND said to stop biotin for 4 days before thyroid labs. No mention of any others. Now after reading this, I’m thinking a full week would be more accurate.