About 29 million American adults, adolescents, and children are on selective serotonin reuptake inhibitors (SSRIs). In many countries globally some 5-10% of the population are on SSRIs. These have become the first-line treatment for depression.
SSRIs can cause sexual dysfunction and emotional blunting in up to half of people, an unclear incidence of sleep disruption, and a rare risk of suicidality, self-harm, and new-onset psychosis.
Getting off SSRIs can cause discontinuation syndrome in 20-50% of people. It is more common, more severe, and lasts longer when people have been SSRIs for years instead of weeks or months. Many of the discontinuation symptoms represent new-onset dysfunction that cannot be explained by the withdrawal of an effective treatment for the pre-existing depression, such as headache, derealization, depersonalization, cramps, gait abnormalities, and “brain zaps.”
This is educational in nature and not medical or dietetic advice. See terms for additional and more complete disclaimers.
My SSRI series led to the conclusion that serotonin’s primary role in the entire body is to coordinate mitochondrial energy production according to shifts in oxygen demand, that SSRIs are primarily mitochondrial drugs, that SSRIs can cause direct and severe mitochondrial toxicity in a small number of people, and that SSRI withdrawal causes new-onset mitochondrial dysfunction in a large number of people.
Many people asked how to transition from SSRIs to using my Depression Protocol, which is a drug-free approach to depression.
What to Do About SSRI Withdrawal Mitochondrial Dysfunction was meant for helping people who experience SSRI discontinuation syndrome or have been experiencing it for a very protracted length. One of its points, however, was that, as long as you’ve been on the drug for more than six to eight weeks, you want the taper to be as slow as possible.
While I am not a medical doctor and cannot manage anyone’s medications, here are some insights derived from the literature about how to make the taper slow, and, most importantly, hyperbolic. Hyperbolic means you don’t go down the same number of milligrams each time; instead, you go down in smaller and smaller increments as you go on.
Mark Horowitz of the Prince of Wales Hospital in Sydney, Australia, and David Taylor of Kings College London Institute of Pharmaceutical Science published a paper on this topic in 2019.
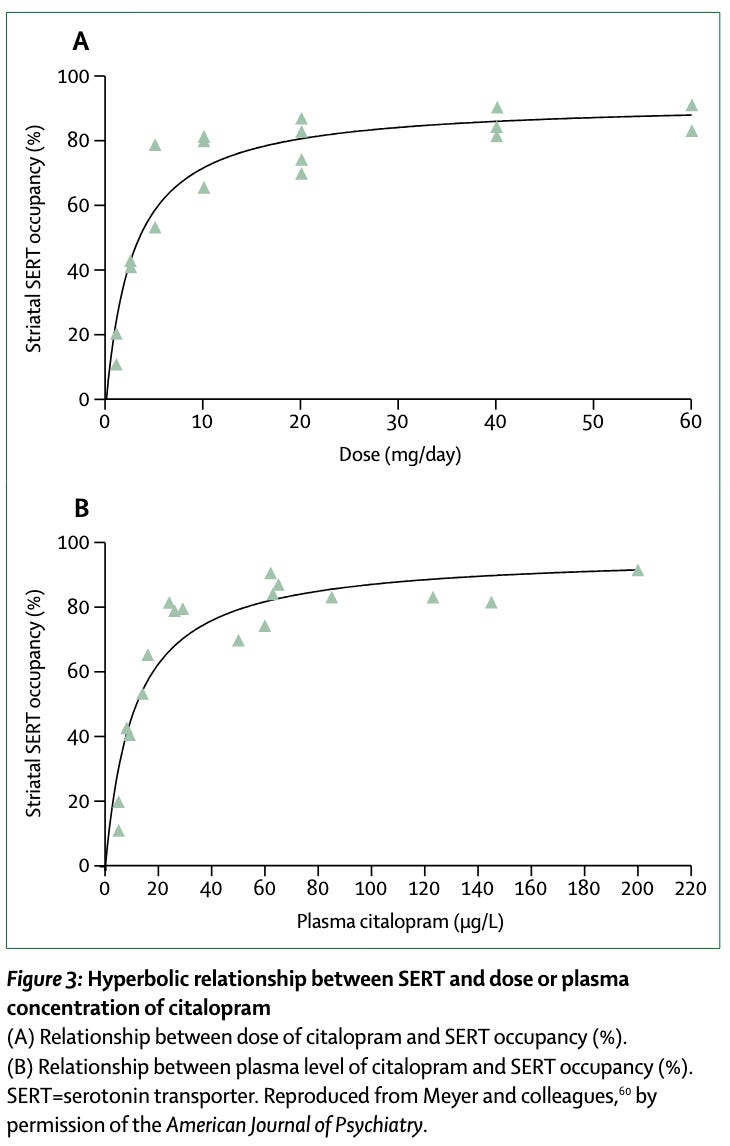
They pointed out that as the dose of an SSRI goes up, the modeled occupancy of the serotonin transporter levels off:
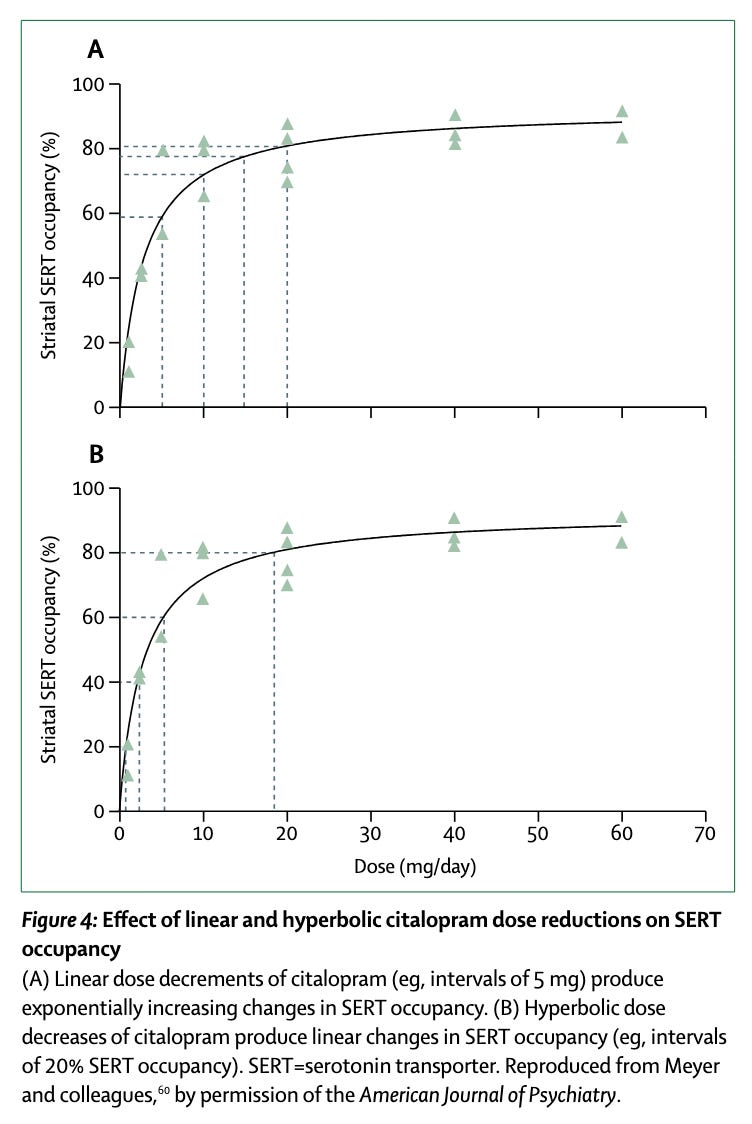
The figure below shows the impact of a linear dose reduction on the top and a hyperbolic dose reduction on the bottom.
When you reduce the dose linearly, your early reductions have a very small impact on transporter occupancy and your later dose reductions have a massive impact.
If you want to achieve a smooth, even reduction in transporter inhibition, you need to make large dose reductions at first, and then progressively smaller and smaller dose reductions as you move on in the taper.
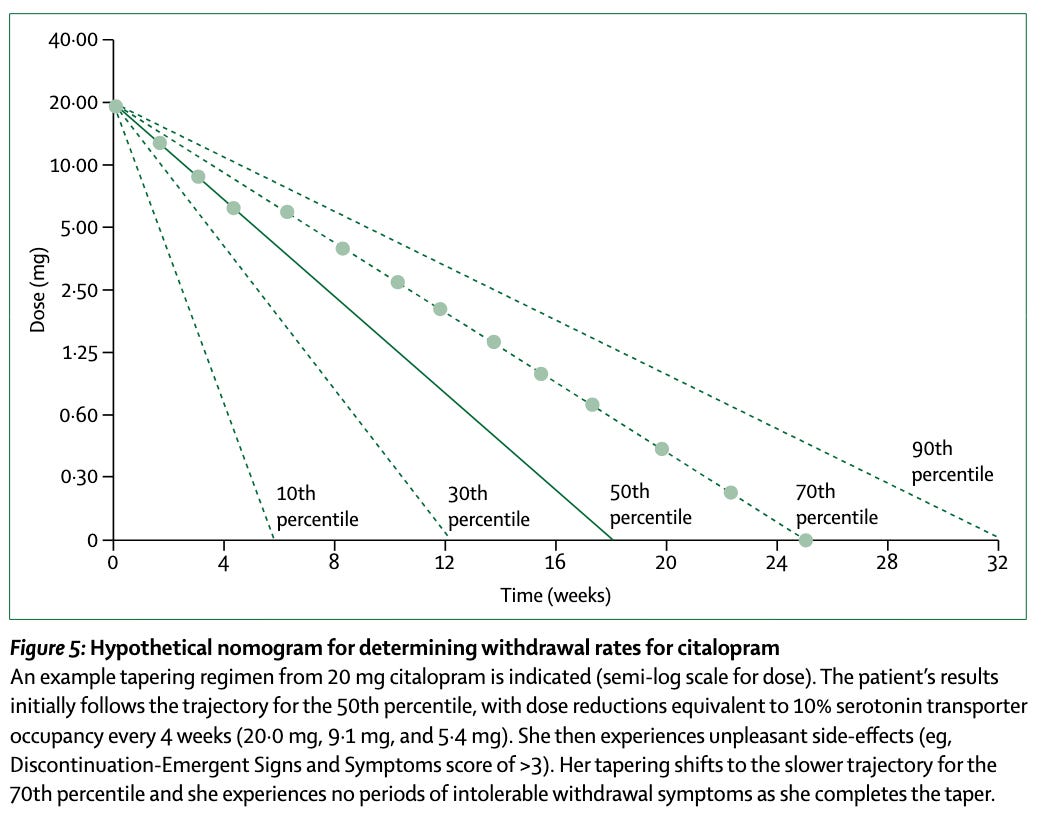
They modeled the range of speeds that could be used, where ten percent of people can taper off in six weeks or fewer, 10 percent of people take longer than eight months, and the median person takes 18 weeks.
In the hypothetical case they gave, the person starts on the median trajectory, but experiences discontinuation symptoms after several dose reductions, so she shifts over to the slower trajectory meant for the 70th percentile.
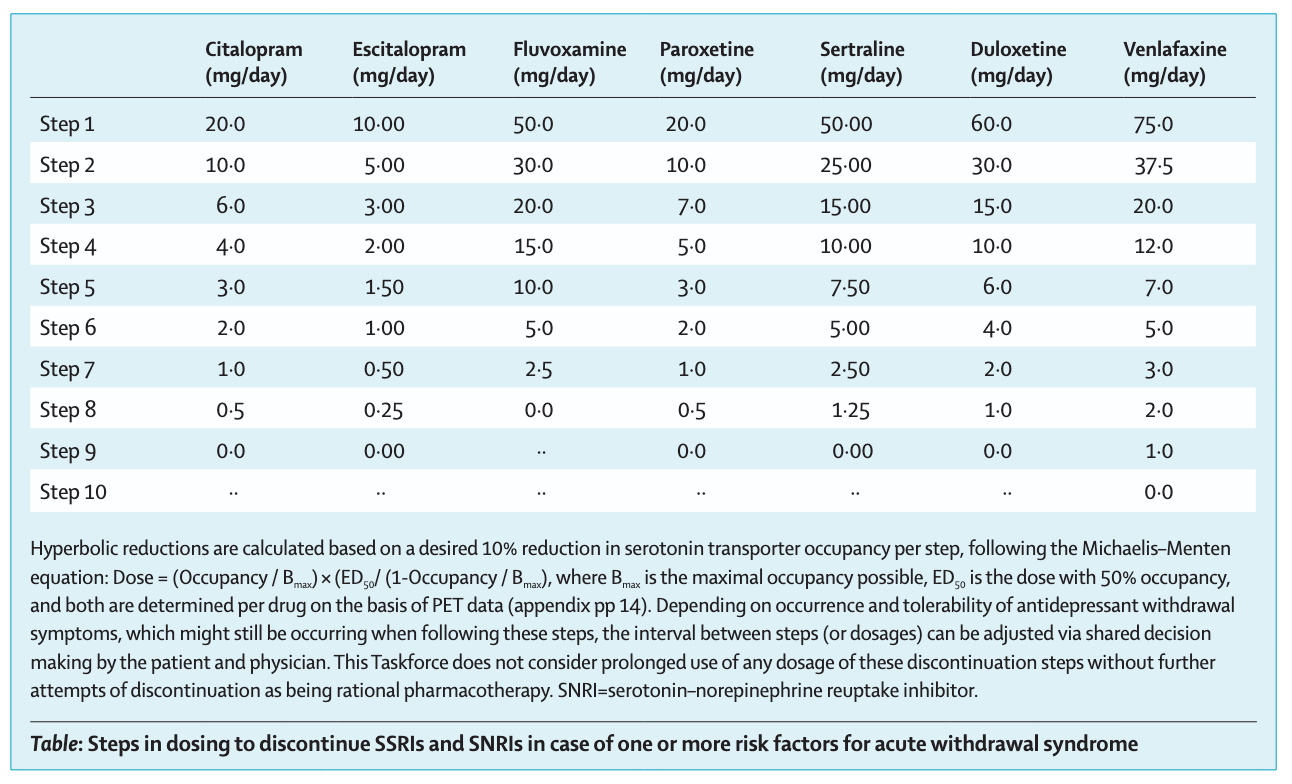
Henricus Ruhe and colleagues of the Dutch Discontinuation of Antidepressants Task Force replied to their paper with a useful table that models 9- and 10-step taper protocols representing 10% reductions in transporter inhibition per step for the various SSRI and SNRIs:
They suggested that one could start with one week per step instead of the slower approach suggested by Horowitz and Taylor. If the patient reports discontinuation symptoms emerging, they can go back to the previous dose and taper more slowly.
Anecdotally, I have heard of some people taking six months per step, dragging out the taper protocol to five years.
Here is my suspicion:
Take up to as long in the taper as you spent on the drug.
This is based on the literature I reviewed strongly suggesting that incidence, severity, and duration of discontinuation symptoms is driven by the time spent on the drug.
Here is a simple way to approach this. I do not give out medical advice so this is an idea you can bring to your physician to help you get off these drugs if you decide to get off them:
Follow the dose reduction pattern in the table.
Make an initial plan for each step to take two weeks.
If you experience new-onset problems as a result of the taper, go back to the dose prior to the emergence of those problems, and switch to a slower taper.
You can also make the increment even smaller. For example, you could model the dose reduction after the next, smaller step. Or if you get to “0” in the table, you can replace it with half of the previous dose.
If you switch to a slower taper you can at first expand it to three weeks, but you should strongly consider taking the entire time you spent on the SSRIs and dividing it by ten. For example, if you have been on SSRIs for eight years, this would be 416 weeks; divided by ten, this makes each step take 41.6 weeks. You could make it simpler by rounding up to 42 weeks, or even just go down one step per year.
If you require a slow taper, you could try the suggestions in What to Do About SSRI Withdrawal Mitochondrial Dysfunction to see if they can improve taper tolerance and allow you to go more quickly.
If you experience a return of depression but not other new problems, you can then use my Depression Protocol for a drug-free approach. In general, it is not contraindicated to mix SSRIs with anything in that protocol, but you should exercise caution with anything else impacting serotonin (e.g. 5-HTP) or monoamine oxidase (dodder, pomegranate, ellagic acid). If you require an extended taper, you should use the the “optimize it” version of the protocol with the assistance of medical supervision as you likely have idiosyncratic mitochondrial dysfunction as either a background vulnerability or as caused by the SSRIs themselves.
Have experience with a successful taper? Post in the comments!


This is very interesting to me as a retired GP, who worked with university students with mental health issues. By about the year 2000, I had realised that SSRI withdrawal reactions could be severe, and the standard advice of withdrawal over a couple of weeks was hopelessly inadequate for those who had been on them a while. I started advising something similar to the protocol you describe, with very gradual withdrawal over many weeks to months, depending on how long they'd been taking them, and the individual response to gradual dose reduction. Sometimes I changed them to fluoxetine, which was available as a liquid and so was more flexible.
The tragedy is that we had very little else to offer people who were depressed. There was some CBT available ( long wait time, restricted number of sessions). It would have been very helpful to have had an alternative approach such as your depression protocol. Thank you for developing it.
I was on Paroxetine for 5 years (18 to 23) and experienced the most horrific life ordeal when I came off of them. Became suicidal, paranoid, extremely stressed etc. I had to use a liquid solution to do so. I did not know how I survived this to be honest. This is what lead me to translate and read the "Walsh Protocol" to French researchers. Following Paxil taper, I fell back into depression and then was deemed "treatment resistant". I had to totally turn my back to conventional medicine, go off sugar, increase magnesium and B6, check my methylation status, read biochemistry a lot. Thanks for your work Dr Masterjohn. Your content is part of what saved my life. SSRI "withdrawal" is greatly underestimated by doctors. This is terrible and no Human should have to ever go through that. Never.