May 25, 2006
(Please also see my more recent and extensive article, From Seafood to Sunshine: A New Understanding of Vitamin D Safety, as well as my article on vitamin D nutrition during pregnancy and lactation, Vitamin D in the Infant: Requirements and Safety.)
One of cholesterol's many functions in the body is to act as a precursor to vitamin D.
Vitamin D can also be obtained from foods. Interestingly, foods that provide this vitamin -- all of which are animal foods -- tend to be high in cholesterol.
Since cholesterol is a precursor to vitamin D, inhibiting the synthesis of cholesterol will also inhibit the synthesis of vitamin D. Since sunlight is required to turn cholesterol into vitamin D, avoiding the sun will likewise undermine our ability to synthesize vitamin D. And since vitamin D-rich foods are also rich in cholesterol, low-cholesterol diets are inherently deficient in vitamin D.
Vitamin D is best known for its role in calcium metabolism and bone health, but new roles are continually being discovered for it, including roles in mental health, blood sugar regulation, the immune system, and cancer prevention. Yet standard modern advice -- take cholesterol-lowering drugs, avoid the sun, eat a low-cholesterol diet -- combined with a recommended daily intake of vitamin D that is only a tenth of what many researchers believe to be sufficient all seems to pave the way for widespread vitamin D deficiency.
Perhaps that's why, according to Dr. John Cannel, President of the Vitamin D Council, most whites and nearly all blacks in modern society are deficient in vitamin D.1
In This Article:
Sources of Vitamin D: Synthesis of Vitamin D in the Skin by Sunlight
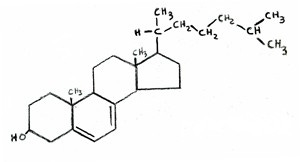
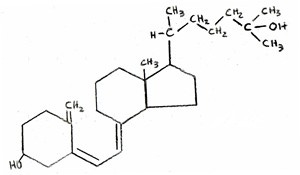
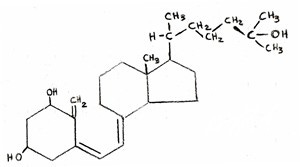
When sunshine in the UV-B spectrum strikes the skin, it converts a substance in the skin called 7-dehydrocholesterol into vitamin D3.2
7-dehydrocholesterol is a very close precursor to cholesterol. If you look at our flow chart showing the synthesis of cholesterol, you will see that it shows lanosterol being converted directly to cholesterol. This conversion is actually believed to take more than 18 different steps and hasn't been completely figured out, so it is usually simplified as one step.3 7-dehydrocholesterol occurs very close to the end of this conversion, so is often referred to as "cholesterol" or "a form of cholesterol."
Figure 1: The Chemical Structure of 7-Dehydrocholesterol
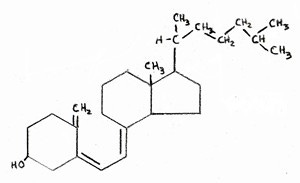
Figure 2: The Chemical Structure of Vitamin D
When atmospheric conditions are ideal and skies are clear, 30 minutes of whole-body exposure of pale skin to sunlight without clothing or sunscreen can result in the synthesis of between 10,000 and 20,000 IU of vitamin D. These quantities of vitamin D are large, and therefore capable of supplying the body's full needs.2
At the same time, the body has two mechanisms to prevent an excess of vitamin D from developing: first, further irradiation converts excess vitamin D in the skin to a variety of inactive metabolites; second, the pigment melanin begins to accumulate in skin tissues after the first exposure of the season, which decreases the production of vitamin D.2
The availability of UV-B rays, however, depends on the angle at which sunshine strikes the earth, making vitamin D synthesis impossible for most people at most latitudes during parts of the year called the "vitamin D winter."4
Outside the vitamin D winter, sufficient UV-B rays for full vitamin D synthesis do not suddenly become available: the window of time during each day in which vitamin D synthesis can occur gradually expands as the season progresses, as does the amount of UV-B radiation available within that window.4
Many different factors can make the availability of UV-B widely variable during any given time of the year. Clouds alone, for example, can eliminate up to 99 percent of UV-B radiation.5
Natural variations in the density of the ozone layer can cause the length of the vitamin D winter to increase or decrease by up to two months. Aerosols and buildings block UV-B radiation, while increased altitude or reflective surfaces such as snow increase exposure to UV-B radiation.5
In the past, researchers suggested that any place outside of 34 degrees latitude experiences some degree of vitamin D winter, that the vitamin D winter in Boston extended for four months from November through February, and that the vitamin D winter in Edmonton extended for six months from October through March.5
More recently, researchers found that so many factors influence the availability of UV-B light that vitamin D winters under some conditions in Boston and Edmonton could be much shorter, whereas under other conditions, vitamin D winters can even occur at the equator.5
Since most of us live at latitudes that are covered by a vitamin D winter for at least part of the year, and since most of us work indoors and wear clothing and sunblock when outdoors in the summer sun, it is necessary for most of us to consume vitamin D in food for at least part of the year, or to supplement with vitamin D.
In order to consume vitamin D as food, we must eat the cholesterol-rich animal foods we are so often told to avoid.
Sources of Vitamin D: Foods High in Vitamin D Are High in Cholesterol
By far the richest source of dietary vitamin D is cod liver oil -- a substance that takes the honor of being the food second richest in cholesterol. At 5.7 milligrams of cholesterol per gram of food, cod liver oil beats out its nearest competitor -- chicken liver -- by 0.09 mg/g, and is one third richer in cholesterol than the notorious egg. It is second only to the expensive delicacy of caviar, which comes in at 5.9 mg of cholesterol per gram.
The second richest source of vitamin D is lard. No, you didn't read that wrong -- lard. Lard ranks #18 on our list of the top 22 foods richest in cholesterol, and is over four times richer in vitamin D than its nearest competitor, herring. Granted, the pigs need to be exposed to sunlight to generate vitamin D.
Other sources of vitamin D include fatty fish, some shellfish, egg yolks, and butter -- foods selected almost entirely from the list of those richest in cholesterol.
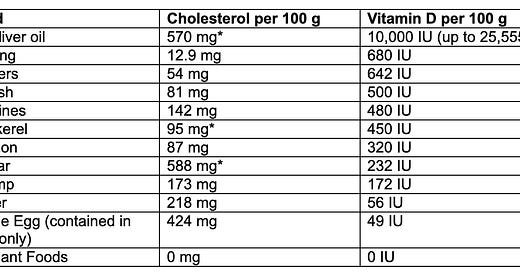
The table below shows the overlap between foods' status as cholesterol-rich and vitamin D-rich.
Table: Dietary Sources of Vitamin D36
The correlation between cholesterol content and vitamin D content certainly isn't perfect, but all of the foods that contain vitamin D contain substantial amounts of cholesterol, and most of the foods high in vitamin D are quite high in cholesterol.
Sources of Vitamin D: Do Plant Foods and Mushrooms Really Contain Vitamin D?
Many "vitamin D" supplements contain vitamin D2, which is obtained by subjecting ergosterol, a chemical found in plants, to radiation.
Recently, news reports declared that mushrooms subjected to ultraviolet radiation are "[zapped] into a giant serving" of vitamin D.7 Like plants, any vitamin D contained in mushrooms is in the form of vitamin D2.8
Should sources of vitamin D2 really be considered sources of vitamin D?
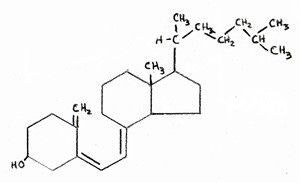
Some researchers claim that vitamin D2, also called "ergocalciferol" and called "viosterol" in the old days, and vitamin D3, also called "cholecalciferol" are equally effective in humans because their ability to bind to the vitamin D receptors in our cells is equal.2 But that's not the whole story.
Figure 3: The Chemical Structure of Vitamin D3 (Cholecalciferol)
Figure 4: The Chemical Structure of Vitamin D2 (Ergosterol)
Vitamin D is carried in the blood by vitamin D-binding protein (DBP). DBP is kind of like a savings account for vitamin D. If you didn't have the DBP, you'd be forced to use all your vitamin D as soon as you absorb it, and excrete the rest. This would be a giant waste of vitamin D, because you can only use so much at a time. DBP thus helps to increase the effect of a given dose of vitamin D by holding on to what you don't need at any given moment for later use, and helps prevent toxicity by keeping the portion you don't need at any given moment from being delivered to your cells.2
Although vitamin D2 binds well to the vitamin D receptor, it has very little affinity for vitamin D-binding protein. For this reason, it is well-known to be useless in chickens and other birds. When vitamin D was seen merely as a cure for rickets, vitamin D2's ability to treat rickets in the small amounts needed led researchers to believe it equal in power to vitamin D3 in humans. Now that researchers are uncovering the need for much higher levels of vitamin D to maintain optimal health, it is becoming clear that vitamin D2 just doesn't fit the bill.
The researchers Laura Armas, Bruce Hollis, and Robert Heaney showed in 2004 that vitamin D2's low affinity for the vitamin D-binding protein makes it nearly ten times less effective at raising long-term vitamin D levels.9
If vitamin D2 has a lower affinity for the DBP, it follows that it is also much more likely to result in toxicity than is vitamin D3. It is therefore unsurprising that, according to Dr. John Cannel, president of the Vitamin D Council, nearly all cases of toxicity from pharmacological doses of vitamin D resulted from the consumption of vitamin D2.10
The vitamin D2 synthesized from plant sterols should therefore not be considered true vitamin D for humans. Humans should obtain vitamin D from the sun and from the vitamin D-rich fatty animal foods that provide the form of vitamin D with which the sun provides us, and which we have consumed throughout our evolution.
The Many Functions of Vitamin D: More Than Just Bone Health and Calcium
Vitamin D is best known for its role in calcium metabolism, especially for its role in the treatment of rickets. Yet modern science is discovering that it has many more important roles, from mental health and immunity to blood sugar regulation and cancer prevention. In fact, there is some evidence that the vitamin D found in those notoriously "artery-clogging" cholesterol-rich foods may help prevent heart disease.
Cod liver oil was first used as a therapeutic agent in the 1770's, and by the mid-1800's it was well-recognized as a cure for the childhood bone disease, rickets, which is marked by an expansion of the bone's metaphyseal plate and a buildup of unmineralized bone matrix, and its adult equivalent, osteomalacia. Upon the discovery of vitamin A in 1913 as a component of cod liver oil and butterfat, researchers assumed vitamin A to be responsible for cod liver oil's ability to cure rickets. In 1921, however, a team of researchers established that there was a separate component of cod liver oil responsible for its ability to cure rickets, which came to be known as vitamin D.11
In the early 1970's researchers discovered that vitamin D is actually activated into an endocrine hormone within the body, and over the course of the 1980s researchers discovered the vitamin D receptor, which is a nuclear receptor for vitamin D that enters the nucleus and alters the expression of genes once vitamin D binds to it.12
Since then, the scope of vitamin D research has broadened immensely. The Vitamin D Council, headed by Dr. John Jacob Cannel, MD, has compiled information on vitamin D's role in the following areas:
Autoimmune illness
Cancer
Chronic pain
Diabetes
Heart disease
Hyperparathyroidism
Hypertension
Mental illness
Multiple sclerosis
Muscle weakness and coordination
Obesity
Osteoarthritis
Dr. Cannel has proposed that a variety of the above conditions be used as indicators for "Vitamin D Deficiency Syndrome," and urges that physicians test the vitamin D levels of patients who exhibit those indicators and treat patients with deficient levels with sunlight or vitamin D supplementation.
Vitamin D Deficiency: Do Cholesterol-Lowering Statin Drugs Inhibit Vitamin D Synthesis?
Researchers know that vitamin D synthesis declines with age -- and so does the concentration of 7-dehydrocholesterol in the skin. Without 7-dehydrocholesterol in the skin, sunlight has nothing to turn into vitamin D. The researchers consider it likely, then, that the decreased synthesis of 7-dehydrocholesterol is responsible for the decreased synthesis of vitamin D that comes with age.2
It follows then, that the cholesterol-lowering drugs known as statins, or HMG CoA reductase-inhibitors, which inhibit the synthesis of 7-dehydrocholesterol, also inhibit the synthesis of vitamin D.
(View our flow chart of the cholesterol synthesis pathway here. )
As of May 25, 2006, there are no studies indexed for Medline that tested the effect of statins on vitamin D levels for longer than three months, and only one, single study out of three that tested the effect of statins on vitamin D levels for longer than one month -- conducted a whopping fifteen years ago. The small handful of short-term studies found no effect.13
By contrast, researchers who showed that statins induce dramatic deficiencies of coenzyme Q10 in humans first retested coenzyme Q10 levels after six months of administering the statin. They further found that coenzyme Q10 levels kept decreasing over time for over 18 months before settling.14
We would expect statins to take even longer to cause a drop in vitamin D levels, because, whereas coenzyme Q10 is measured directly in the blood, the 7-dehydrocholesterol takes time to migrate to the surface of the skin and accumulate there. So what is the effect of statins on vitamin D levels one year down the road? Two years? Five? Ten?
The truth is we have no idea, because no one has bothered to study it.
Vitamin D Requirements: How Much Do We Need?
Although the U.S. RDA for vitamin D is a mere 400 IU, modern research is showing that much higher levels are needed to maintain adequate vitamin D status for optimal health.
After vitamin D is obtained from the diet or absorbed from the skin, it is semi-activated to 25 (OH) D or 25-hydroxyvitamin D in the liver. This is the primary storage form of the vitamin that is carried by vitamin D-binding protein in the blood. As needed, 25 (OH) D in the blood is fully activated to 1, 25 (OH)2 D or 1, 25-dihydroxyvitamin D -- called calcitriol -- in the kidney primarily in response to low calcium levels.
The skin also has the ability to produce small amounts of activated vitamin D, and most of the tissues in the body have the capacity to activate vitamin D when stimulated to do so by the immune system -- completely separate from the calcium-regulated system that governs vitamin D activation in the kidney.2
It is the 25 (OH) D form of vitamin D that is considered the valid test of one's nutritional vitamin D status. If you ask your doctor for a vitamin D test, make sure your doctor orders the 25 (OH) D test and not the 1, 25 (OH)2 D test.
Figure 5: The Chemical Structure of Vitamin D
Figure 6: The Chemical Structure of 25 (OH) D
Figure 7: The Chemical Structure of 1, 25 (OH)2 D
In order to maximize calcium absorption, blood levels of 25 (OH) D need to be maintained at 30 ng/mL, which, in the absence of UV-B light, would require roughly 2600 IU per day of vitamin D. The risk of fracture continues to decline at even higher 25 (OH) D levels because people with higher vitamin D levels actually fall less often, suggesting a neuromuscular benefit to high levels of the vitamin. Even higher levels of 46 ng/mL are needed to maximize the body's ability to regulate blood sugar, and since dark-skinned agricultural workers in the tropics have 25 (OH) D levels of about 60 ng/mL, it's probable that this is closer to the ideal level.15
The researcher Robert Heaney showed that people use about 4,000 IU of vitamin D per day when they are running on storage deposits of the vitamin,15 suggesting that this is the amount we should be consuming from food or supplements during a vitamin D winter.
Since many of us do not get full-body skin exposure even during the summer, and wear sunscreen when we do, it is probably ideal for most of us to consume some lesser amount of vitamin D even during the warmer months.
Dr. Cannel of the Vitamin D Council recommends testing your 25 (OH) D levels periodically if you consume more than 2000 IU of vitamin D just to be on the safe side. He says he personally takes 5,000 IU during the winter, 2,000 IU during the early spring and late fall, and none in the months in between.16
The Toxicity of Vitamin D
In 1997, the Food and Nutrition Board of the U.S. Institute of Medicine set the limit for the amount of vitamin D that was guaranteed safe to take at 2000 IU per day. According to the vitamin D researcher Robert Heaney, "the vitamin D content experts on the Upper Limits Panel objected to this 2000 IU/day figure on the grounds that extensive clinical experience had established the safety of substantially higher inputs," and several other investigators have since called for the Institute of Medicine to raise the upper limit.15
According to Heaney, extensive sun exposure produces vitamin D levels equivalent to taking 10,000 IU per day, from which no dangers have ever been observed.
Worse, the upper limit set by the Institute of Medicine is lower than the dose that many people need to take simply to gain sufficient levels of vitamin D. "It would be difficult," wrote Heaney, "to make a policy recommendation to provide the amounts needed for a major sector of the population in the face of [an upper limit] that remained as low as 2000 IU."15
The vitamin D researcher Reinhold Veith wrote a review in 1999 asserting the safety of 10,000 IU of vitamin D per day and challenging the medical community to produce any evidence for the widespread assumption that doses under 10,000 IU could be toxic.10
In 2001, Ian Monroe, the chair of the Institute of Medicine's committee on vitamin D toxicity wrote in praise of Veith's work and promised that it would be taken into account at a future meeting of the Institute, but this has yet to happen.
Dr. Cannel searched the literature for case reports of toxicity from pharmacological doses of vitamin D3. Although he found cases of vitamin D2 toxicity, he found only one, single case of vitamin D3 toxicity: one man took vitamin D supplements for two years that were mislabeled, containing up to 430 times the amount of vitamin D as was listed on the label. He took between 156,000 IU and 2,604,000 IU per day for those two years, and "recovered uneventfully after the proper diagnosis, treatment with steroids and sunscreen."10
(You can read his report on vitamin D toxicity here. )
Vitamin D Safety — Make Sure You Get Your Vitamin A
Animal studies show that vitamins D and A each protect against toxic effects of the other -- suggesting that vitamin toxicity might be more a result of vitamin imbalance than vitamin excess.
In humans, supplementation with vitamin D appears from case reports to allow the average 75-kg human to take an additional 175,000 IU of vitamin A per day before vitamin A toxicity symptoms begin to develop.17
Vitamin D increases the need for vitamin A in chickens even in small amounts that are insufficient to guarantee freedom from rickets. One study showed that massive doses of vitamin A alone caused bone and growth problems in turkeys, while massive doses of vitamin D alone caused kidney problems -- yet when these doses were combined, the turkeys exhibited no signs of toxicity at all.17
Since most foods that are high in vitamin D are also high in vitamin A, it makes sense to either consume those foods that provide both, or, if one is to take high doses of vitamin D, to also supplement with vitamin A -- or to take a supplement that provides both, such as cod liver oil.
Likewise, if one is eating vitamin A-rich foods or taking vitamin A supplements, one should also make sure one is getting enough vitamin D.
Without Cholesterol, There Is No Vitamin D
Cholesterol's connection to vitamin D is intimate. It is the synthesis of cholesterol that ultimately provides for the synthesis of vitamin D, and it is cholesterol-rich foods that provide the dietary sources of vitamin D during times of the year when it is impossible for us to make our own.
Vitamin D is not one more reason to consider cholesterol good for the body. The days when vitamin D is seen as a unifunctional vitamin reponsible simply for calcium metabolism and bone health are quickly disappearing into the annals of history. Vitamin D is quickly being recognized as a hormone with myriad important roles in the body -- and thus credit for each of those benefits of vitamin D falls back on its close relative and precursor, cholesterol.
The lesson? Lots of sunshine and cholesterol-rich foods are good for you. If you skip the cholesterol and take vitamin D supplements, make sure they are vitamin D3 and not vitamin D2 -- and you can thank our favorite molecule that provided the precursor for the vitamin D in your supplement.
References
1. Cannel, John, "Vit D: When Why Where and How Much," Wise Traditions 2005 November 12, 2005 (lecture).
2. Adams and Hollis, "Vitamin D: Synthesis, Metabolism, and Clinical Measurement." In: Coe and Favus, eds., Disorders of Bone and Mineral Metabolism, Philadelphia: Lippincott Williams and Wilkins (2002) p. 159.
3. Champe et al., Biochemistry: 3rd edition, Philadelphia: Lippincott Williams and Wilkins (2005) p. 219.
4. Webb, et al., "Influence of season and latitude on the cutaneous synthesis of vitamin D3: exposure to winter sunlight in Boston and Edmonton will not promote vitamin D3 synthesis in human skin," J Clin Endocrinol Metab, Vol. 67 No. 2 (1988) 373-8.
5. Engelsen, et al., "Symposium-in-Print: UV Radiation, Vitamin D and Human Health: An Unfolding Controversy: Daily Duration of Vitamin D Synthesis in Human Skin with Relation to Latitude Total Ozone, Altitude, Ground Cover, Aerosols and Cloud Thickness," Photochemistry and Photobiology, 81 (2005) 1287-1290.
6. Unless accompanied by an asterisk, cholesterol facts are from USDA Nutrient Facts, Standard Release 17, http://www.nal.usda.gov/fnic/foodcomp/Data/SR17/wtrank/sr17a601.pdf and vitamin D facts are from Sullivan, Krispin, "The Miracle of Vitamin D," http://www.westonaprice.org/basicnutrition/vitamindmiracle.html#food Accessed May 24, 2006. An asterisk indicates the fact is obtained from NutritionData: "Nutrition Facts Calorie Counter," http://www.nutritiondata.com. Accessed May 24, 2006.
7. MSNBC: "Light-zapped mushrooms filled with vitamin D," http://www.msnbc.msn.com/id/12370708/. Published April 18, 2006. Accessed May 24, 2006.
8. Jasinghe, et al., "Bioavailability of vitamin D2 from irradiated mushrooms: an in vivo study." Br J Nutr, Vol. 93 No. 6 (2005) 951-5.
9. Armas, et al., "Vitamin D2 Is Much Less Effective than Vitamin D3 in Humans," The Journal of Clinical Endocrinology and Metabolism, Vol. 89 No. 11 (2004) 5387-5391.
10. Cannel, MD, John Jacob, "The Truth About Vitamin D Toxicity," http://www.vitamindcouncil.com/vitaminDToxicity.shtml. Published September 4, 2003. Accessed May 24, 2006.
11. Rosenfeld, Louis, "Vitamine - vitamin. The early years of discovery," Clinical Chemistry, Vol. 43 No. 4 (1997) 680-685.
12. DeLuca, Hector F., "Historical Overview," in Feldman et al., eds., Vitamin D, San Diego: Academic Press (1997) 3-11.
13. Dobs, et al., "Effects of pravastatin, a new HMG-CoA reductase inhibitor, on vitamin D synthesis in man," Metabolism, Vol. 40 No. 5 (1991) 524-8.
14. Folkers, et al., "Lovastatin decreases coenzyme Q levels in humans," Proc Natl Acad Sci USA Vol. 87 No. 22 (1990) 8931-4.
15. Heaney, Robert P., "The Vitamin D requirement in health and disease," Journal of Steroid Biochemistry & Molecular Biology, 97 (2005)13-19.
16. Cannel, MD, John Jacob, "The Vitamin D Newsletter: April 2006 -- Dr. Cannell Answers Readers' Questions," Vitamin D Council: http://www.vitamindcouncil.com/PDFs/April2006-questions.pdf. Published April 1, 2006. Accessed May 25, 2006.
17. Masterjohn, Chris, "Vitamin A on Trial: Does Vitamin A Cause Osteoporosis?" Wise Traditions, Spring 2006.