September 10, 2007
Much of the illusion that cholesterol causes disease may be due to a molecule called Rho. Rho is part of the stress response. Once it is activated, it makes sweeping changes to the shape and tension of the cell, causing the assembly of vast "actin stress fibers" that stretch across the cell and allow it to contract.1
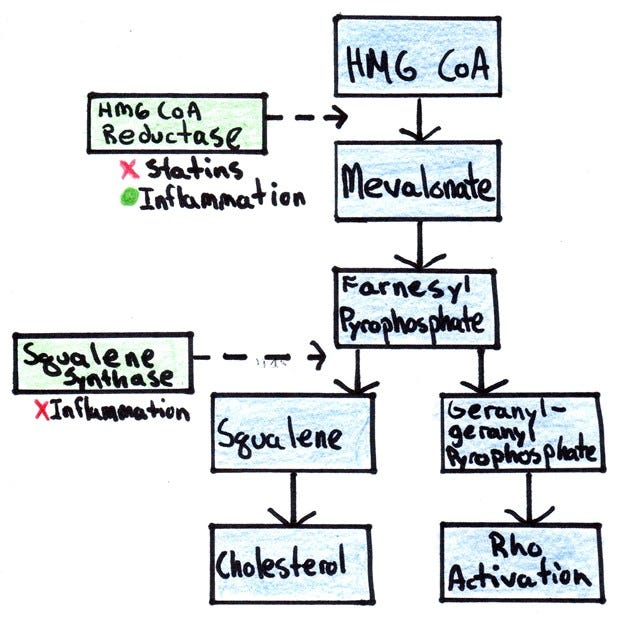
As shown in the figure below, the key signal that activates Rho — geranlygernayl pyrophosphate, or GGPP — is a product of the cholesterol synthesis pathway.
Statins Do More than Lower Cholesterol
The medical establishment and media have caused a great deal of confusion by referring to statins as "cholesterol-lowering drugs."
Statins inhibit the synthesis of mevalonate. As my general chart of cholesterol synthesis shows, this results in the inhibition of not only cholesterol, but coenzyme Q10 and various isoprenes that are responsible for attaching sugars to proteins and proteins to membranes as well.
Rho Activation Correlates with Cholesterol
Since statins inhibit the synthesis GGPP, they also inhibit the activation of Rho.
But it doesn't end there. Statins inhibit both GGPP and cholesterol through the same mechanism: the inhibition of mevalonate. Thus, the ability of a particular statin or a particular dose of statin to inhibit cholesterol is going to correlate with its ability to inhibit the activation of Rho.
Inflammation Increases Cholesterol Levels and the Activation of Rho
The figure above also shows that inflammation increases the synthesis of mevalonate but decreases the synthesis of squalene. The result is that cholesterol increases somewhat, but much more mevalonate is left over for the activation of Rho.
When researchers feed hamsters endotoxin — a pro-inflammatory chemical released from the breakdown of bacterial cell walls — mevalonate production increases ten-fold, while cholesterol increases only two-fold.2
This means that high cholesterol may be a marker for chronic infection in many people — but that the more important factor leading to disease could be the activation of Rho.
Why would the activation of Rho cause disease?
Rho Activation Causes Disease by Inhibiting Nitric Oxide Synthesis
It turns out that Rho's assembly of stress fibers doesn't come without its casualties. When Rho gets switched on, it severely suppresses the production of the enzyme endothelial nitric oxide synthase (eNOS), which synthesizes nitric oxide.3
Nitric oxide is a gas that relaxes and dilates blood vessels, increasing the flow of blood; decreases the adhesion of white blood cells to the lining of the vessel walls; inhibits the migration of smooth muscle cells to the sites of atherosclerotic lesions; and decreases the formation of blood clots.
In other words, nitric oxide might be our primary bulwark against atherosclerosis.
Atherosclerosis — It All Comes Down to Nitric Oxide
In fact, these effects of nitric oxide can even explain why blood vessels wind up with atherosclerotic lesions in some specific places and not others. Nitric oxide production increases when the blood vessel lining is exposed to shear stress — that is, when blood runs parallel to it. When blood flow is disturbed, blood also runs perpendicular to the lining, causing a decrease in nitric oxide production. Atherosclerotic lesions occur primarily at sites where blood flow is disturbed.4
High cholesterol levels may be a marker for something far worse — chronic over-activation of Rho. And cholesterol lowering with statins may be a marker for something far better — inhibition of the activation of Rho.
Waging the War the Right Way
We have spent decades laboring under the illusion that when the cholesterol concentration in the bloodstream increases beyond a critical point, it just begins caking up the pipes. Naturally, we concluded that to wage war against heart disease, we must wage war on cholesterol.
A more fruitful battle plan would be to attack the cause of the problem itself — inflammation.
References
1. Wojciak-Stothard B, Ridley AJ. Rho GTPases and the regulation of endothelial permeability. Vasc Pharmacol. 2003;39:187-199.
2. Memon RA, Shechter I, Moser AH, Shigenaga JK, Grunfeld C, Feingold KR. Endotoxin, tumor necrosis factor, and interleukin-1 decrease hepatic squalene synthase activity, protein, and mRNA levels in Syrian hamsters. J Lipid Res. 1997;38:1620-1629.
3. Laufs U, Liao JK. Post-transcriptional Regulation of Endothelial Nitric Oxide Synthase mRNA Stability by Rho GTPase. J Biol Chem. 1998;273(37):24266-24271.
4. Libby P. Inflammation and cardiovascular disease mechanisms. Am J Clin Nutr. 2006. 291:803-816.