Now that Donald Trump and RFK Jr. have launched a national discussion about the role of seed oils in health, and now that Kennedy has been hazed into the presidential cool kids club by eating seed oil fries on Trump Force One, it’s time to talk about seed oils.
Is RFK right that we should make frying oil tallow again?
If you have an X account, please repost this there where it will have the most influence:
Seed oils are high in polyunsaturated fatty acids (PUFAs), which have two or more double bonds, and are uniquely vulnerable to a process called lipid peroxidation, during which they are broken down into small, toxic byproducts that cause cellular damage.
I explained the chemistry behind this unique aspect of PUFAs here. I also covered it in my Antioxidant Course.
Lipid peroxidation plays a role in most chronic diseases. It damages DNA, which contributes to cancer. It damages lipoproteins, which contributes to heart disease and inflammatory liver disease. It damages proteins in whatever tissue it occurs, contributing to neurodegenerative disease, or Hashimoto’s thyroiditis. Lipid peroxidation in pancreas can contribute to diabetes and in the hypothalamus it can contribute to obesity.
Lipid peroxidation is not deterministically driven by seed oil intake. Rather, the PUFAs in seed oils are uniquely vulnerable to it, and many other factors determine the production and clearance of oxidants that could cause damage to them. Eating seed oils increases the whole-body burden of PUFAs and thus the vulnerability to lipid peroxidation.
Seed oils tend to be high in vitamin E because plants need vitamin E to protect themselves against lipid peroxidation. In the short-term, seed oils will increase vitamin E status. However, vitamin E follows PUFAs wherever they go in the body, and it has a shorter half-life than those PUFAs. As tissue burden of PUFAs increase, the vitamin E requirement goes up, and eventually seed oils can increase the demand for vitamin E more than the supply.
Seed Oil Trials Need to Be Long
Data we will look at below shows this takes about four years to balance out. This is one among several reasons that short-term trials lasting weeks can be deeply misleading.
Another problem is that if your tissue burden of PUFAs increases, whether this leads to harm is contextual on your total oxidant burden and your antioxidant status. Various behaviors (smoking, drinking, overeating), many environmental exposures (heavy metals, pesticides, herbicides), and most chronic disease states can increase oxidant burden. The biggest problem is that aging itself increases oxidant burden and we all get older.
This is another reason short-term studies can be misleading: in a randomized trial you aren’t going to see the negative effects on, say, cancer risk, unless a) the tissue burden has been given long enough to maximize, b) long enough time for the disease process has been given to play out and c) the people are old enough to get cancer in the first place.
As I explained here, people mostly don’t get cancer until they become old enough to get it.
Seed Oils and Fatty Liver
Another case where this applies is in fatty liver disease. Numerous short-term trials have shown that substituting seed oils for more saturated fats increases liver fat in humans. None of these trials have produced diagnosable fatty liver, but they have shown relative increases in liver fat within the healthy range.
The problem is that the most important harm of fatty liver is the inflammatory destruction that occurs in the advanced stage known as nonalcoholic steatohepatitis (NASH), where lipid peroxidation is responsible for cirrhosis, fibrosis, cancer, and even death due to liver failure. This takes time to play out.
If we synthesize the human trials with the more numerous and mechanistically insightful animal experiments, we find that the increase in liver fat that occurs when eating saturated fat would be abolished with sufficient protein or choline and that seed oils are necessary for the progression to the much more dangerous NASH.
I explained this and cited the relevant research here.
I further criticized the simplistic treatment of short-term human trials here.
Seed Oils and Heart Disease
Where seed oils have been studied the most is in the context of heart disease. In this case we have numerous randomized controlled trials lasting five to eight years.
We will spend most of the rest of this article analyzing those trials. First, though, some brief comments on the much less useful observational studies.
Heart Disease: Observational Studies
A meta-analysis of 13 prospective cohort studies found that those with the highest PUFA intakes were 15% less likely to develop heart disease than those with the lowest intakes.
One of the problems with these studies is that the earliest any were published were in 1996. The earliest studies included collected data in 1986 (PMID 8688759) and in 1985-1988 (PMID 9149659).
By this time, there had already been a global public health campaign exhorting the population to replace traditional fats and oils with seed oils to prevent heart disease. The apex of this campaign was in 1984, when the NIH Consensus Conference dubbed high cholesterol as the cause of heart disease based on a trial with a cholesterol-lowering drug, cholestyramine.
Time Magazine proclaimed, “Hold the eggs and butter – cholesterol is proved deadly, and our diet may never be the same.”
Among their dietary advice was to replace eggs, organ meats, cheese, butter, bacon, beef, whole milk, coconut oil, and palm oil with corn, safflower, soybean, and sesame oils.
That is, to replace animal fats and tropical oils with seed oils.
This all came stamped with the authority of the US Federal Government and “the broadest and most expensive research project in medical history.”
The problem with collecting data on PUFA intake starting in 1985 is that now everyone has become profoundly biased toward believing that if they replace animal fats and tropical oils with seed oils they will prevent heart disease.
This then selects for people who are committed to increasing their health and who tend to believe what their society is telling them is the best way to meet their goals.
This, then, leads to “healthy user bias.” That is, people who are health-conscious are doing all sorts of things to improve their health that are tangled up with the behavior whose causation you are trying to study.
The meta-analysis cited above adjusted the data for total energy, age, smoking, body mass index, physical activity, education level, alcohol intake, hypertension, fiber intake, and percent of energy from SFAs, trans fat, monounsaturated fatty acids (MUFAs), alpha-linolenic acid (ALA), PUFAs other than LA and ALA, and protein intake.
If we condense the fatty acid composition into one variable, this is an adjustment for 11 items.
Is it the case that this behavior is mostly confounded by 11 things?
I could easily rattle off dozens of things that are likely to impact the risk of heart disease. For example, antioxidant nutrients will directly interact with PUFA intake but none of them were adjusted for here, not even vitamin E!
The idea that you can adjust your way into unconfounded associations in observational studies is driven by a lack of epistemological humility. If you believe that the 11 items you have identified are most of what there is to know, adjusting for them should yield an unconfounded result. If you believe that there is a lot more you don’t know than that you do know, the idea of adjusting them into an unconfounded result is ridiculous.
For example, someone who switches to seed oils after the launch of a government-backed health campaign is probably both conscientious and agreeable. Even these psychological traits themselves are associated with disease risks. Conscientiousness is lower in people with heart disease (PMIDs 36362545 and 37297784), and both agreeableness and conscientiousness are associated with healthier blood pressure patterns (PMID 24608035).
Heart Disease: Randomized Controlled Trials
We can get better insights by looking at long-term randomized, controlled trials (RCTs). When trials are large enough, randomization equilibrates not only the known confounders, but also the much larger group of unknown confounders between groups.
Meta-analyses of these trials have come to different conclusions depending on which trials they include and which questions they ask.
For example, one commonly cited meta-analysis found seed oils associated with a 19% lower risk of heart disease, quite similar to the 15% lower risk found in prospective cohort studies.
On the other hand, Christopher Ramsden’s group produced two meta-analyses (PMIDs 21118617 and 21865817) arguing that both randomized trials and prospective cohort studies show that omega-3 oils are protective and omega-6 oils harmful.
My own position is that these trials are so heterogeneous that meta-analyzing them is intrinsically misleading, and the heterogeneity involves a LOT more than the balance of omega-3 and omega-6 oils.
First of all, some of the “RCTs” in this meta-analysis are not even randomized.
Second, many of them changed all kinds of things besides the type of oil being consumed.
Third and finally, the most important trial of all time, the LA Veterans Administration Hospital Study, cast doubt on the other trials for being too short and in people who were not old enough to detect the cancer risk.
The two estimates in the middle for men and women in “Finnish” represent the Finnish Mental Hospital Study. This was NOT a randomized controlled trial.
The Finnish Mental Hospital Study followed a model where there were two hospitals. And for a period of about five years, they had Hospital A eat a lot of PUFA and Hospital B eat a lot of saturated fat. And then after that they switched them for another five years so that the hospital that was getting PUFAs is now getting saturated fat and vice versa.
Well, that’s not a randomized controlled trial, because the unit of randomization was the hospital. But if that’s the case, then each group had one hospital in it. How do you do statistics with an N of one? You can’t. The people in the hospitals weren’t randomized to anything. So you can’t analyze the risk of the individuals and call it a randomized controlled trial if what you randomized was one hospital to each group of hospitals.
Oslo, DART, and STARS should be removed for being too multifactorial. Removing these three removes 37% of the data!
Removing them with Finish removes 54% of the data!
Here are the main problems with them:
Two important trials were excluded: Rose 1965 and Sydney Diet-Heart.
Rose 1965 did not reach statistical significance, but heart disease was higher on corn oil than what people had been naturally eating.
Sydney Diet-Heart found 39% worse total mortality in men who had myocardial infarction, and amusingly concluded that men who have had myocardial infarction “are not a good choice for testing the lipid hypothesis.”
Only two of the trials were double-blind and placebo-controlled, and we should give these two trials more weight than the others.
These represent 32% of the data.
Since we removed 54% of the data that doesn’t belong, these two trials should be nearly our exclusive focal point.
The Minnesota Coronary Survey was the one trial included that found a higher risk of heart disease with seed oils, according to the plot.
Minnesota had two important traits besides being double-blind:
It was by far and away the largest trial, having almost ten thousand people in it.
It was the only trial that included women, and about a third of the subjects were women.
Ramsden uncovered never-before-published data from this trial and published it in 2016 (PMID 27071971).
These newly recovered results showed:
The greater the drop in cholesterol, the greater the total mortality.
This total mortality effect was driven by people over 65. In that group, a 30 mg/dL drop in cholesterol predicted a 35% greater risk of total mortality.
In autopsies, evidence of heart disease was twice as high in the seed oil group.
The effect on total mortality in over-65ers will become very important when we consider the other double-blind trial, the LA Veterans Administration Hospital Study.
It is the only trial where the mean age was over 60. It was also the longest trial, lasting over eight years.
Here is the design:
On the surface, the results showed seed oils decreased heart disease mortality but increased mortality from everything else combined:
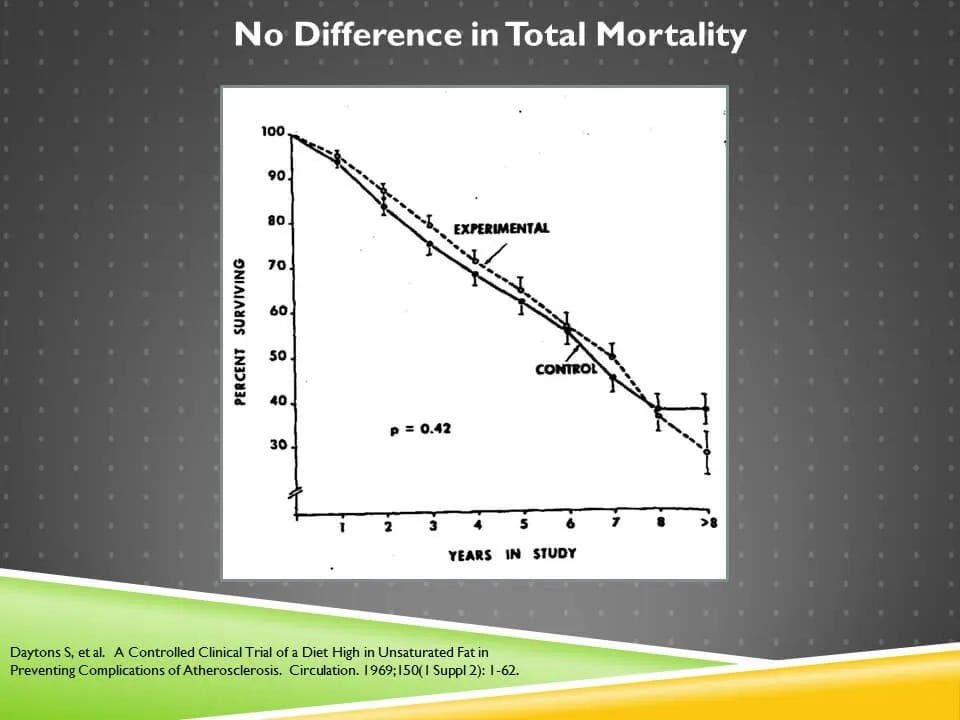
The net effect is there was no difference in total mortality (“experimental” is seed oils):
One concerning thing is that you can see the two lines separating at the 8-year mark, where total mortality favors the control group. This raises the question: would total mortality have begun diverging to become statistically significant after eight years?
In an analysis of cancer, the groups diverge at the 2-year time point, broaden apart in the 3-5-year time point, and really start separating after six years. The result just barely missed statistical significance, but appear to favor seed oils causing cancer.
When non-CVD death was tracked over time, it takes seven years to start separating in favor of seed oils increasing total mortality.
The general trend here is that the initial benefit to CVD fades over time, while the increase in cancer and non-CVD mortality takes hold after many years.
One of the major confounders was that there were more moderate and heavy smokers in the animal fat group.
Smoking should increase risk of both heart disease and cancer, so the fact that the heart disease benefit was temporary in the seed oil group and they still had a long-term increase in cancer looks much worse when we find out that heavy and moderate smoking was concentrated in the animal fat group.
Further, the mix of fats in the animal fat group seems particularly nefarious. The vitamin E content was even lower than that found in commercial butter, and it would have been massively higher if the subjects were eating grass-fed butter.
Since vitamin E prevents lipid peroxidation, which plays a role in both heart disease and cancer, and since smoking raises the vitamin E requirement (PMID 16814530) this again looks like the animal fat group was severely handicapped and still beat the seed oil group overall.
In fact when CVD was looked at stratified by smoking, all of the excess cardiovascular death in the animal fat group occurred in the moderate and heavy smokers.
This is strong evidence that smoking on the background of a vitamin E-deficient diet drove the cardiovascular harm, and that this confounding is the only reason the cardiovascular results differ from those of the Minnesota Coronary Survey.
The fact that cancer still occurred in the seed oil group then really looks bad, because the confounding was so heavily favoring cancer rising in the animal fat group.
Thus the two double-blind trials when looked at together suggest:
Seed oils when controlled properly increase the rate of heart disease.
The vitamin E content of seed oils can protect against the cardiovascular harms of vitamin E deficiency and moderate to heavy smoking, but only over the short-term.
Seed oils increase the risk of cancer and total mortality, but you need a population over 60-65 to see it.
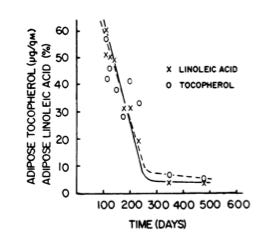
The LA Vet study showed that it takes years for the tissue PUFA content to plateau:
Animal studies show that vitamin E concentrations hug tightly to the tissue PUFA content (PMID 4951506).
In human data only published as a conference abstract and reviews (PMID 4572178) – so take this with a grain of salt – vitamin E levels increase with seed oils for 1.7 years but even out with traditional oils by four years.
While I can’t put much faith in the data just described, it makes complete sense because the vitamin E turnover is higher than the PUFA turnover, and the PUFA saturation takes four years to plateau, so around the fourth year is when the supply and demand of vitamin E due to seed oils reach an equilibrium.
This could explain why in the LA Vet study, the cardiovascular benefit of the vitamin E got lost over time and gave way to the cancer risk.
So, the best quality evidence suggests that seed oils increase the risk of heart disease and cancer, that you need trials to be longer than eight years to see the full effects, and that deviations from these trends can be explained by confounders such as smoking and vitamin E.
More broadly, we know that most nutrients play some role in protecting against oxidative stress so there are far more interactions to uncover than just smoking and vitamin E. But these are sufficient to reconcile the findings of the two double-blind RCTs.
Seed Oils and Obesity
Now, do seed oils cause obesity?
The bodyweight results from the LA Vet study suggest not:
However, the seed oil group (“experimental”) generally spent most of the trial having ever so slightly higher bodyweight than the animal fat group, and while this collapsed in years six and seven, it ended with that slight difference intact.
Given the complexity of lipid peroxidation, it should be regarded as a hypothesis worthy of much more investigation that lipid peroxidation in the hypothalamus could hurt energy balance, with the acknowledgment that there are lots of contextual factors that will determine the effect.
It may be that this is more important during early development, or that it is more relevant in free-living subjects where they have more choices to consume more hyper-palatable food.
Further, it could be that foods in 2024 are much more hyper-palatable than those in the 1960s, and that moderate hypothalamic damage from an interaction between long-term seed oil intake and oxidants could put one at a disadvantage in wading through the morass of hyper-palatability.
A Closer Look at Cancer
One critique of the cancer risk in the LA Vet study is there were more people who had “low adherence” among those who died of cancer.
Note that these people DIED of cancer. “Adherence” was defined by the number of meal tickets punched in the dining hall. Not whether the people are safflower oil instead of butter. Cancer decreases appetite, especially if it kills you.
So this is undoubtedly at least partially explained by fatal cancer decreasing food intake.
Overall, though:
1) The rigorous analysis sticks to what is randomized. Adherence isn't randomized. The solid randomized finding is that CVD benefit gets lost over time and turn into an increased cancer risk.
2) While the lowest adherence group has 5x the cancer in the seed oil arm, even in the highest adherence group there is 3x the cancer in the seed oil arm, and only a third of the cancer is concentrated in the lowest decile adherence. If you remove the lowest decile adherence you still have 40% more fatal cancer in the seed oil arm.
3) If you were to posit it's all due to low adherence you are left with a really weird trend: why did it take years for the cancer trend *difference* between the groups to emerge and why did it keep separating over time if this is a result of randomness?
Randomness on average favors null effects and not clear time dependent trends. The data overall look far too "logical" to be random.
The best explanation is that as vitamin E status declined and tissue PUFA saturation maxed out, lipid peroxidation drove an increase in cancer risk, with some portion of the adherence difference due to cancer decreasing food intake.
Should We Make Frying Oil Tallow Again?
Should we make frying oil tallow again?
This issue is more complex than it appears on the surface.
Inside the body, tallow has practically no ability to undergo lipid peroxidation. However, in repeatedly reheated frying conditions, any oil can peroxidize.
Soybean oil is actually more stable than tallow in these conditions.
However, grass-fed tallow is much higher in vitamin E and other antioxidants. (PMID 20219103).
Rather than simply proclaiming a national recommendation to replace seed oils with tallow in restaurant fries, RFK Jr. as Secretary of HHS should call on the research community to test fryer oil stability in different traditional fats including tallow produced under different conditions, including grass-feeding, and with various natural, flavorful antioxidants added for protection.
He should also call on the research community to more thoroughly investigate the potential role of seed oils in obesity, especially from a perspective of hypothalamic damage.
Given the role of seed oils in promoting heart disease and cancer, though, I am happy with the rallying cry to make frying oil tallow again to bring attention to this issue as we move toward a more open-minded and nuanced take about how to Make America Healthy Again.
If you have an X account, please repost this there where it will have the most influence:


























Great research here as always, but honestly... I dont think switching the type of oil restaurants use to deep fry food is something that gobs of money and energy should be spent on. I could think of a long list of things that seem more impactful to focus on to turn around health, as I am sure many of you can also. But here is where I should probably just divest and say I really dont think a government, let alone the one in this country, has ever operated in a way OR WILL ever operate in a way that has the optimal health of its 'people' in its highest regard. Nonsense. No saviours there, and we should not be looking at a government to save us. If you want to eat fries that are fried in tallow, make them at home yourself or get some community members to rally and urge your local restaurants to switch. This top down stuff is just not the way to go imo. I could say more...Ill keep to this for now.
All said, Chris Masterjohn really does offer good research and food for tbought, so thanks!
Absolutely yes!!!
But it needs to be grass fed tallow.
So we have to switch all cattle raising to regenerative methodologies all across the country.
There’s not much point in switching to a tallow that is contaminated with glyphosate, GMO residue, antibiotics and vaccines that industrial raised cattle are given.
We must put first things first, and change the way we are raising the cattle so what they yield is healthy meat, tallow and bones for broth.
It sounds like a big undertaking, but the reality is the federal government is subsidizing industrial agriculture to such a large extent that when the direction is given that subsidies will only go towards regenerative agriculture, the industry will change very quickly.
First things first.
Make America Healthy Again